Secondary consultations would improve access to specialists
by Peter Breadon
Getting a specialist referral from your GP can feel like bad news, and not just because the specialist might give you an unwelcome diagnosis. Too often, it means a long, anxious wait to get care, or a huge fee after you get it.
Many reforms are needed to make sure all Australians can get the specialist care they need. But good systems for secondary consultation – where GPs can easily get advice from non-GP specialists – is among the quickest and easiest fixes. It’s time to roll them out in every state.
As previously reported, our new Grattan Institute report shows that the specialist care system – if you can even call it a system – is broken.
There are nationwide shortages of some types of specialists, including psychiatrists and dermatologists. In some communities, there are shortages of most types of specialist care. Wait times for public care are often far too long, and the fees for private care can be outrageously high.
We propose reforms that span from training to investment, and that need action from specialist colleges and the federal and state governments. Some are politically hard or costly. But one solution is surprisingly cheap and easy, and it’s already starting to get traction.
Explaining secondary consultation
Secondary consultation is a doctor-to-doctor discussion about a specific patient question. GPs ask a question and share relevant patient information. Non-GP specialists then provide detailed recommendations on diagnosis and care, or advise that a referral is needed.
It happens all the time, but it’s scattershot. GPs typically rely on their personal network, which overseas-trained GPs in Australia often lack. It’s hard to line up a free slot in two busy doctors’ schedules. And at the moment neither doctor is directly paid for their time on the phone.
All that means it’s often easier for GPs to simply refer a patient onwards than to get advice that might save the patient the delay and cost of seeing another doctor.
There have been many schemes to make secondary consultation easier. But they have mostly been limited to a single region, only focused on one specialty, and lacked ongoing funding.
We looked at bigger, broader systems that give GPs secure, text-based advice.
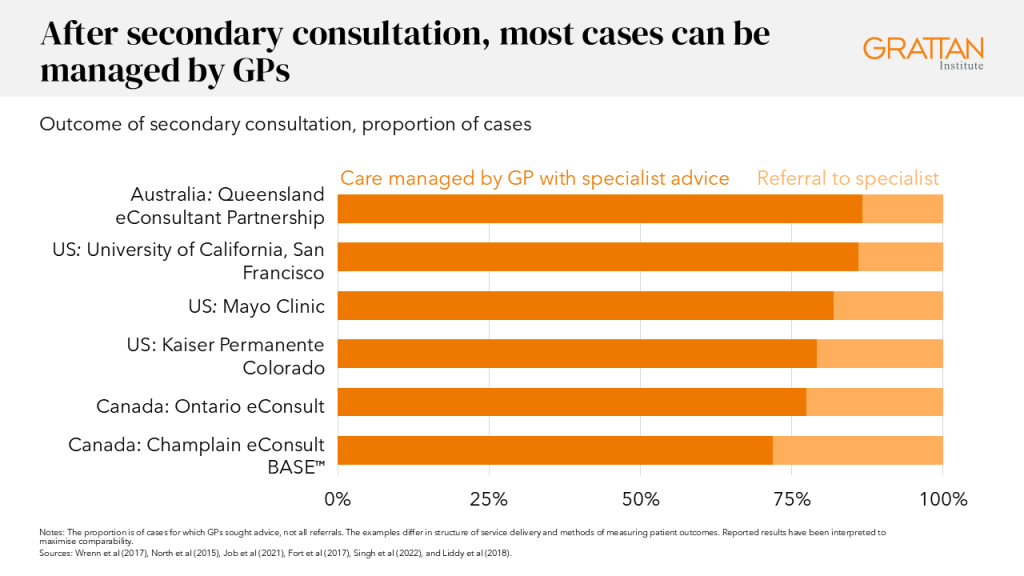
In the US, Canada, and parts of Australia, these systems resolve 70-to-90 percent of cases in primary care without needing a referral.
There are other valuable ways to do secondary consultation, ranging from video calls to joint consultations with patients.
But text-based systems don’t need busy doctors to be available at the exact time, making it the most practical and efficient model for questions that don’t require in-depth, real-time discussion.
Many of these systems share some key ingredients:
- Timely advice, within three days
- High-quality advice, with qualified specialists providing responses, and monitoring of referral rates, turnaround time, and GP satisfaction, to make sure the system is working
- One door to many specialties, so that GPs can use it often without switching between systems
- Covering doctors’ costs, with funding for GPs and the specialists providing advice.
Our modelling shows that 140,000 consultations a year could avoid about 68,000 unnecessary referrals and save patients about $4 million in out-of-pocket fees.
It would only cost governments about $26 million a year. That’s a rounding error in health budgets, but it would free up scarce specialist slots for people who really need them.
Gaining traction
Queensland began piloting this approach in 2021. Evaluations found that it’s clinically safe and popular with GPs. The Crisafulli Government recently committed ongoing funding, expanding the program to cut waitlists and support rural and remote GPs.
That shifts the model from a promising pilot to a permanent part of the system – the digital equivalent of opening new outpatient clinics, but without bricks, mortar, or long drives for patients.
Across the Nullarbor, secondary consultation was a 2025 election commitment. In February, the WA Government pledged $8.2 million for a “GP ASK” secondary consultation pilot covering five high-demand specialties.
The Royal Australian College of General Practitioners welcomed the promise, saying it could help relieve crowded specialty waiting lists and emergency departments.
Time to go national
If Queensland has already moved from try-out to roll-out, and Western Australia is about to join the club, why should patients in NSW, Victoria, Tasmania, South Australia, or the Territories keep waiting?
Health Ministers could pool lessons from Brisbane and Perth, agree on national design principles, and set a deadline: by 2027 every Australian GP will have digital access to specialist advice within three days.
Secondary consultation won’t fix every problem in our specialist system, but it’s a rare reform that delivers faster care, fairer access, and lower costs in one click. The technology is proven, the costs are small, and the need to tackle waiting times and specialist fees has never been greater.
It’s time to move from pilots to policy, and put specialist advice on every GP’s desktop.