How the federal government can tackle low vaccination rates in aged care
by Peter Breadon
If your parent is in aged care, you hope they can have a fulfilling life and get all the support, compassion, and companionship they need. At a minimum, you expect they will get basic healthcare.
But three years after a Royal Commission uncovered widespread failures in Australia’s aged care, new figures show the treatment of our vulnerable elderly remains shameful.
In December last year, only 31 percent of aged care residents had been vaccinated for COVID in the previous six months. In those six months, more than 1,800 people in Australia died from COVID, most of them older people.
Meanwhile, in England, more than 80 percent of care home residents were up to date with their COVID vaccines in time for Christmas.
Australia’s aged care vaccination rate has improved since then. But a resident’s chance of being vaccinated is still close to a coin toss, with only 52 percent vaccinated in the past six months.
In the middle of this year, the rate in England was 68 percent, and in Ireland it was 80 percent.
Data published
In June, the federal Department of Health and Ageing started publishing data on vaccination rates for individual aged care homes, a step we had recommended.
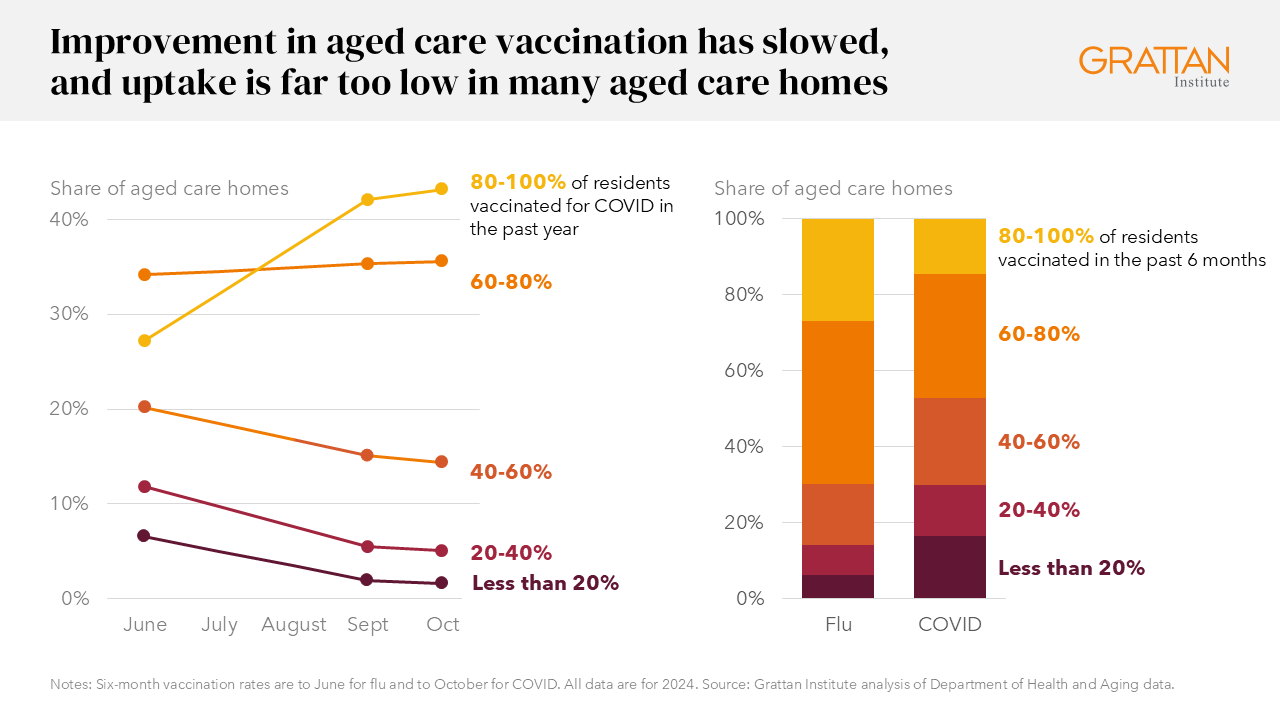
The first data only showed how many residents had been vaccinated over the past year. But the next data, for September and October, showed how many residents were vaccinated in the past six months. That gives us the best picture yet of how aged care homes are performing – and the results are troubling.
More than 1,000 aged care homes across Australia – about 40 percent – have had less than half their residents vaccinated for COVID in the past six months.
Three hundred have less than 10 percent vaccinated, representing more than one in 10 aged care homes.
Aged care homes with these shockingly low vaccination rates are in every state and territory.
Flu vaccination rates are higher, but they’re also nowhere near good enough.
More than 500 aged care homes had less than half their residents vaccinated for flu in the six months to June this year, and more than 100 had less than one in 10 residents vaccinated.
Public reporting of vaccination rates for aged care facilities is welcome, and it seems to have helped, at least at first.
The only measure released for June, September, and October is the COVID vaccination rate for the past year. From June to September, the share of facilities with low vaccination rates plunged.
Action needed
But that progress didn’t go far enough, and now it has stalled. One-year vaccination rates are still increasing slightly, reflecting gains made more than half a year ago.
But from September to October, the share of aged care homes with low six-month vaccination rates edged higher.
More action is needed. People in aged care are older, and often frail. An infection is much more likely to send them to hospital or the morgue.
To make further, faster progress, the Federal Government should do four things.
First, monthly government reporting of aged care-home vaccination rates should be expanded to cover flu, shingles, and pneumococcal vaccines. After taking into account their age and other factors, people in aged care are less likely to get shingles and pneumococcal vaccines than other people.
Second, the Government should set targets for aged care vaccination, covering all adult vaccines. Primary Health Networks, the regional bodies responsible for improving primary care, should be required to help aged care homes to meet them.
Third, the Government should ask the expert body that sets vaccination rules to make them more flexible in aged care. For example, people in aged care should be eligible for COVID vaccinations less than six months after their last vaccine. That is the rule in the UK, and it makes it easier to vaccinate many residents in one visit.
Finally, the Government should improve the star-rating system for aged care that was introduced in 2022. It has been criticised for setting a low standard and not being a good guide for potential residents and their families.
The system is being evaluated, and a new version should include rates of vaccination at each facility, as well the proportion of residents getting GP and allied health care.
No excuse
Three years ago, the Royal Commission found that too many aged care residents were missing out on healthcare, despite needing it more than most people.
Residents have told the independent monitor on Royal Commission implementation that little has changed since then, and he’s called for meaningful reform.
Some reform is happening, including new funding for GPs who provide ongoing care for aged care residents. More reforms are needed, and they will often be costly and difficult to implement.
But vaccination should be the easiest healthcare gap to fix.
Older Australians deserve much better than a 50-50 chance of getting a flu or COVID vaccination simply because of where they live.
These four steps would cost almost nothing and would save lives, meaning there is no excuse for inaction.