Published at The Conversation, Wednesday 5 March 2014
Public hospital spending has been the single fastest-growing area of government spending over the past decade. As governments, policymakers and economists put health spending under the microscope, it’s becoming increasingly clear that continuing the present trajectory is not an option.
Grattan Institute’s report Controlling costly care: a billion-dollar hospital opportunity, released today, shows that improving efficiency in Australian public hospitals could save taxpayers nearly A$1 billion a year.
Cost variation
Grattan’s study identifies significant variation in the costs of treating patients, after adjusting for their illnesses and other legitimate factors. The graph below illustrates how the cost of laparoscopic cholecystectomies – a type of gall bladder removal – differs depending on where it happens.
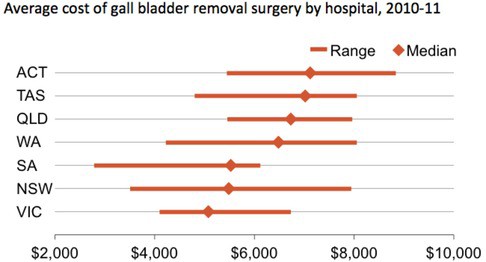
Grattan Institute analysis
Any type of procedure will be slightly different from case to case. But overall, the costs of laparoscopic gall bladder removal surgeries should be expected to be quite similar.
Despite this, costs vary dramatically. In Queensland, the median hospital removes gall bladders for around $6700, while in Victoria the median hospital does it for around $5000. Within NSW, the hospital with the highest cost is more than twice as expensive as the hospital with the lowest cost.
These differences don’t seem to be caused by how many of these procedures a hospital does. Among the five hospitals that do the most, median costs range from less than $4200 to almost $8000.
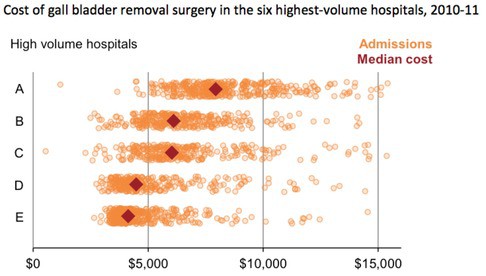
Grattan Institute analysis
Each dot in the graph above represents a different patient, and the costs of their treatment. Each hospital has a considerable spread in costs. But what is important is that for hospitals D and E there is a very different pattern from the others, namely that the distribution of costs for their patients is spread around a lower average and the spread is somewhat tighter.
Potential savings
As the gall bladder surgery example shows, there are big differences in cost structures among states – they have different industrial agreements and different arrangements for purchasing supplies, for example. But the study also shows even bigger differences among hospitals within each state.
These differences can be substantially reduced, though there isn’t a simple fix that will work everywhere. In some cases patients might be kept in hospital longer than necessary. Other hospitals might be paying higher-than-necessary prices for supplies.
Some variation will be legitimate, and caused by factors we don’t yet measure well. But there is no sign that providing better care is one of these. The number of adverse events – the things that go wrong during hospital stays – don’t go down as costs go up.
In our study, we assume that half the variation in costs in any state – after taking into account all measurable factors such as the patient’s condition – is acceptable. Even using that conservative measure, $1 billion of cost is unaccounted.
We estimate that efficiency gains in public hospitals could save taxpayers nearly $1 billion a year.
Driving efficiency
States should use the way they pay hospitals to improve their efficiency.
In 2011, all states and territories and the Commonwealth agreed to a broad strategy to make public hospitals more efficient. All states are now moving to introduce activity-based funding, a formula that pays hospitals at the average current cost of care.
Activity-based funding does provide an incentive for more expensive hospitals to reduce their costs. It is a huge improvement on earlier funding models, but it has one flaw: it’s based on an average that includes hospitals that are spending far too much.
Instead, the price should be set at the average, but after excessive costs are excluded. Such an approach is achievable – it is based on costs that many hospitals are already meeting – and it will improve hospital efficiency.
The second step required to improve the efficiency of public hospitals is to give them information about whether they are more or less efficient than their peers. Comparative information will help them identify the precise areas where they need to improve.
Are they inefficient across the board or only in particular specialties, such as orthopaedic surgery? How does an expensive hospital compare in terms of its staff mix, the number of pathology tests per patient or the cost of supplies? Information on these issues can help hospital managers work out where change needs to occur.
Finally, price signals set by the states need to bite. In the past, price signals to hospitals have been undermined by bailouts – end-of-year government payments to help hospitals balance their books.
State health departments need to keep a close eye on hospital performance, tracking deviations from expected spending. If things go slightly awry, there might be a light touch intervention. But persistent deficits require big measures, up to dismissal of the hospital board, where appropriate.
Demands on the public hospital system are increasing. New technologies become available almost every day. If new needs are to be met, old needs must be met efficiently to create room for new spending.
The Controlling costly care report identifies where money can be saved. Now is the time to phase in implementation of a new funding model to keep the health system sustainable into the future.