As we celebrate International Women’s Day, we should acknowledge that women continue to find it harder than men to get healthcare.
Australia has a universal healthcare system, yet Australian women often pay more than men out of their own pockets for healthcare services.
Why? It could be due to maternal healthcare costs, and the fact that more women than men have multiple chronic conditions. About 55 per cent of Australians with two chronic conditions are women, and about 60 per cent with three or more conditions are women.
Women tend to use healthcare services much more than men. For example, 80 per cent of women saw a GP in 2020-21, compared to 63 per cent of men, and 62 per cent of women received a prescription, compared to 37 per cent of men.
Because they use healthcare services more, women are more likely to face higher healthcare costs over time. And if people have higher healthcare costs, they are more likely to have to defer or skip the care they need.
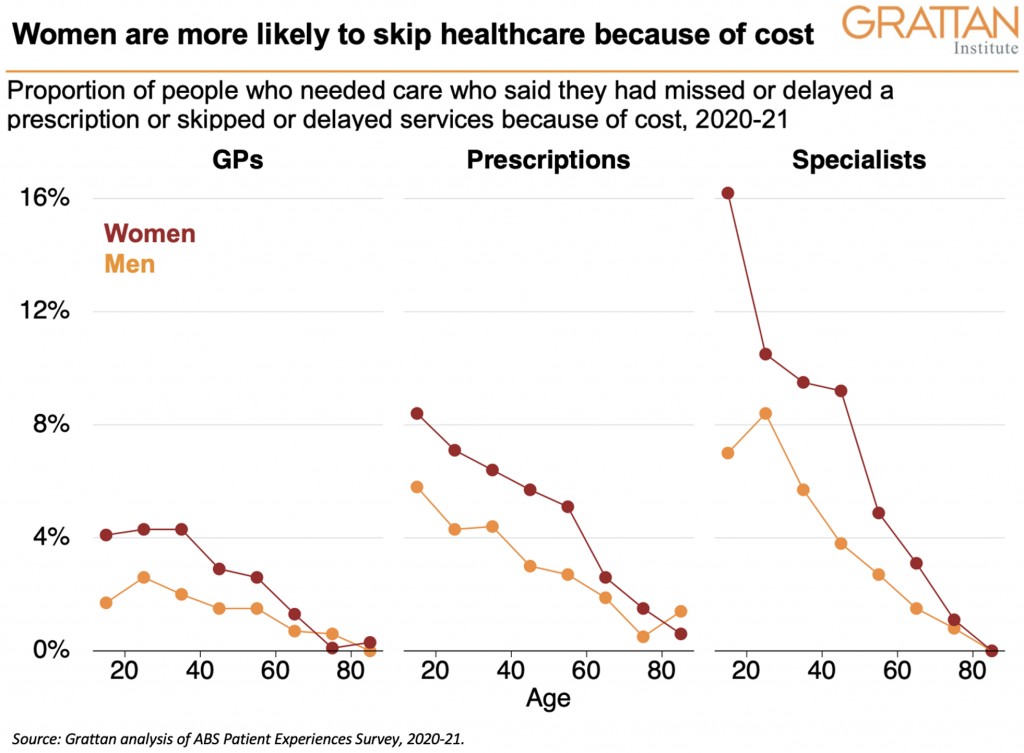
Women are nearly twice as likely than men to skip or delay healthcare because of cost. For example, on average, nearly 8 per cent of women who need specialist care skip it because of cost, compared to 4 per cent of men. This gender divide is also evident for GP services, and prescriptions, as this chart shows.
The average out-of-pocket payment for a Medicare-subsidised service has increased by 50 per cent over the past decade. As healthcare costs increase, the gender divide will only widen.
State and federal governments must act now to reverse this trajectory. We’ve identified many things they can do, in our latest report, Not so universal: How to reduce out-of-pocket healthcare payments.