Summary
The National Disability Insurance Scheme (NDIS) is failing many disabled Australians who need the most support. About 43,500 people with intensive support packages are seeing little benefit from a scheme that was supposed to give them greater choice and improved independence.
Download the accessible text version
The only option for many of these people with profound disability is to live in group homes – where they are at high risk of violence, abuse, neglect and exploitation.
The costs of supporting these 43,500 people is at least $15 billion per year, with average costs per resident of more than $350,000. That’s almost 40 per cent of the total costs of the NDIS for only 7 per cent of its users. Governments need, and disabled people deserve, far better services for this price tag.
Last year’s reports from the Disability Royal Commission and the NDIS Review called for significant reform and a wider range of housing and support services. But neither report provided a clear and detailed roadmap to improve people’s safety and give them alternative options.
There are better and cheaper alternatives to group homes, but they are not widely available, in part because NDIS policies are too rigid and its funding too inflexible. Other countries, including the UK, the US, and Canada, have successfully reformed disability housing and introduced new living arrangements which offer people greater choice and a more individualised approach.
Four big changes are needed to improve housing and support for Australians with intensive needs.
First, the National Disability Insurance Agency (NDIA) should give more support to alternative options, such as those that are working well in Western Australia and overseas, and help more disabled people into ordinary housing in the community.
Second, the current group-home model should be reformed so people who want to share their support can choose who they live with and control how services are provided in their home. Larger group homes should be phased out within 15 years.
Third, the funding process needs to be reformed so people who need intensive support at home get more help to understand their options and navigate the system. People should get early access to an NDIS-funded budget that they can use flexibly, within an overall funding envelope that is affordable for government.
And fourth, the NDIS regulator should step up to ensure the people who depend on these services are safe and have real choice. Specific practice standards should be developed for shared housing and individualised living, with mandatory inspections to make sure the standards are being met and the residents are safe.
Creating more options and better help for people to choose housing and living supports would be a win-win. It would transform the lives of Australians with the most profound disabilities, and it can be done efficiently to help make the NDIS more sustainable for future generations.
Getting this right should be a litmus test for any government seeking to get the NDIS back on track.
Recommendations
1. Create innovative alternative housing and support options, to increase choice and improve sustainability
- Foster a new category of ‘semi-formal’ supports such as home-share and hosts, that enable more individualised living arrangements within current budgets.
- Establish a new housing payment for people with intensive housing and support needs leaving group homes, or who do not qualify for current specialised housing. People could use the money to help them to live in ordinary community homes.
- As an incentive to establish more efficient housing arrangements, allow people to keep any money they save and use it to buy other supports and services.
2. Reform group homes so that people sharing support have more autonomy
over their home life
- Improve the training of staff in shared accommodation, to maximise residents’ quality of life.
- Ensure residents can make collective decisions about how their households are run, by mandating governance arrangements that put the residents in control.
- Require enforceable service agreements in shared accommodation, and require the separation of housing and support so people can choose or change their support provider without putting their tenancy at risk.
3. Improve planning, budget setting, and service coordination
- Create a dedicated pathway for eligible people that streamlines assessment processes and gives people timely access to a consistent budget before planning commences.
- Introduce specialised housing and living navigators, to help people develop their plans, choose their supports, and navigate the system.
- Establish regional hubs to steward the market and commission services. Each hub should have a dedicated fund to accelerate innovation and support promising approaches.
4. Increase guardrails and accountability
- Require all providers of housing and living supports to register. Introduce random inspections of their services, and report regularly on their performance.
- Produce better data on people’s living arrangements as they transition out of group homes.
- Develop specific practice standards for shared accommodation and individualised living arrangements, and conduct inspections to make sure the standards are being met and the residents are safe.
Chapter 1: Disability housing and support is failing those who need it most
One of the NDIS’s most important responsibilities is to provide support to Australians with disability who need extensive help at home with everyday activities. Yet many people who get this support from the NDIS get care that is unsafe and low-quality – despite eye-watering cost.
Many people with profound disability who aren’t in their family home live in group homes, where they share supports with other disabled people. Often they have little say over who they live with or how their support is provided, and too frequently they are subjected to violence, abuse, and neglect.
The NDIS promised more choice and innovation in services, but since it was introduced more than a decade ago, little has changed in the lives of people with profound disability. We need to do better, and we can.
This report lays out why reforming housing and support for these Australians is so important, and what government needs to do to improve current services while creating better, safer, and more sustainable options.
1.1 Disabled Australians with the highest needs rely on the NDIS for housing and support
In 2013, the National Disability Insurance Scheme (NDIS) was set up to provide funding and support to people with significant and permanent disabilities.1 These supports are critical for disabled people to lead independent lives as members of the Australian community.
Some people need very high levels of support from the NDIS to live at home. Many disabled people will never require this level of support.
Figure 1.1: Who receives intensive living support?
| A small group… | typically with intellectual disability… | and intensive needs… | who need significant support. |
|---|---|---|---|
| People with intensive living support funding make up about 7% of the people in the NDIS | 34% of people with intensive living support funding have an intellectual disability | Active support for more than 8 hours per day and some level of support for other hours, including overnight | Payments to people with intensive housing and living support represent at least 37% of the total cost of the NDIS |
This may be because they are able to live independently with a lower level of support, or because family or friends give them significant help. Our focus in this report is on improving the lives of those Australians who require intensive housing and living support in their home.
People who receive intensive living supports (described in Figure 1.1) typically need eight hours or more of help with daily activities such as bathing, getting dressed, going to the bathroom, preparing food, and eating. They also need some form of support to be available overnight in case of emergencies.
The NDIS provides supports to these Australians through several different funding streams. About 33,500 receive Supported Indepen- dent Living (SIL) funding for shared, in-home supports (as shown in Figure 1.2), often in group homes. Another 10,000 receive a similar amount of assistance with daily life (eight or more hours a day) outside of the SIL category.2
About 22,000 people (mostly from the Supported Independent Living cohort) also receive funding for Specialist Disability Accommodation. This money is to pay for specially designed or modified housing, such as housing that is fully wheelchair accessible or has strengthened ceilings for hoists.
The remainder of people receiving intensive NDIS living supports do not receive funding for Specialist Disability Accommodation because they live with their family and have not requested it, because their home does not need enough physical modifications to qualify for it, or because they are not eligible for it. Many group homes, particularly older ones, do not attract significant, or any, Specialist Disability Accommodation funding.3
About 34 per cent of people receiving intensive living support have an intellectual disability. Another 11 per cent have autism, about 10 per cent have psychosocial disability, and about 9 per cent have cerebral palsy or acquired brain injury. The remaining quarter have conditions including multiple sclerosis, spinal cord injury, and other physical and neurological disabilities.4
People with intensive living support who don’t have access to Specialist
Disability Accommodation face many of the same challenges as other Australians in finding affordable housing, with rental affordability at a record low.5 Public and social housing waiting lists are long, and housing stress is high and increasing, particularly among people on low incomes.6
Figure 1.2: People with Supported Independent Living in their plan are more likely to live in Specialist Disability Accommodation housing
NDIS participants by funding category, December 2023
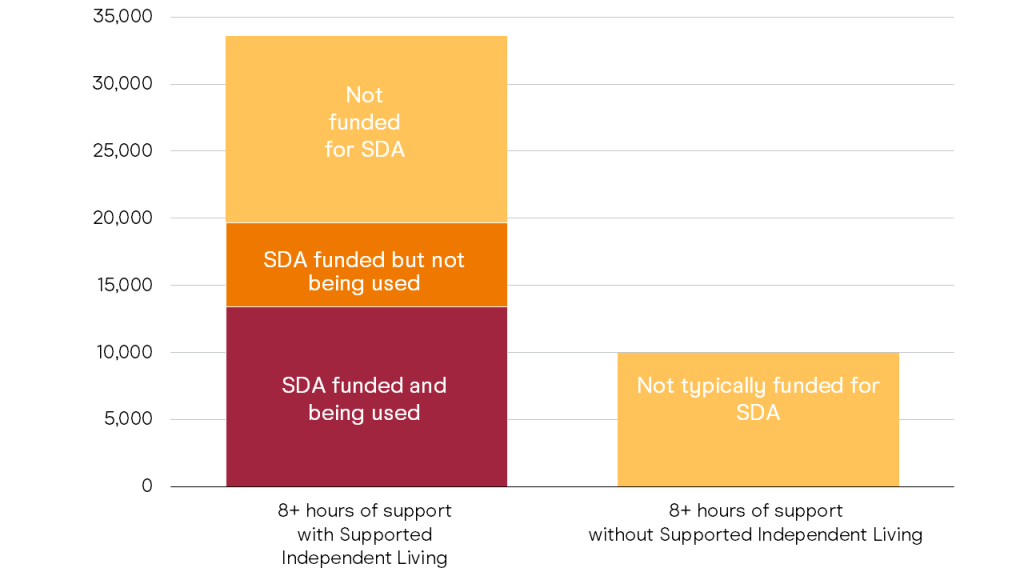
Source: Grattan Institute analysis of NDIS data.
1.2 Despite 10 years of the NDIS, too many Australians still live in group homes
It’s most common for people with Supported Independent Living (SIL) packages to live in group homes. These are houses where support is provided for several people under one roof. Many group homes have three or four residents, while some (known as ‘legacy stock’) have six or more people living together.
A group home is not strictly defined by the number of people living there, but rather the institutional culture that characterises many of these arrangements. Group homes often operate more as service facilities than as homes for their residents.
There are 3,302 group homes across Australia that are registered as Specialist Disability Accommodation, with a capacity of more than 14,000 residents.7 Thousands more people live in group homes that don’t attract Specialist Disability Accommodation funding.8
People who live in group homes tend to stay there for a long time. Nearly four out of five people have lived in their group home for decades, having transferred into the NDIS from old state-run disability systems.9
Little has changed for these people since the start of the NDIS, a scheme that should transform the lives of people with profound disabilities.
1.2.1 Many group homes are low-quality and unsafe
Group homes were governments’ favoured housing and support approach for people with severe disabilities when care was moved out of large-scale institutions.10
De-institutionalisation was led by agencies responsible for disability services, which meant that the focus of housing design was driven by the aim of maximising the potential for those services to be shared.11 Housing multiple residents together enabled providers to more easily organise support-worker time, and manage costs by maintaining some economy of scale in service delivery.12
But the more people who live in a group home, the more difficult it is to create a home-like environment and the higher the safety risk.
Instances of abuse perpetrated against group home residents13 are sadly not isolated and have marred the landscape of disability support for generations.
The Disability Royal Commission heard extensive testimony that showed violence, abuse, neglect, and exploitation is common in group homes.14 The NDIS Quality and Safeguards Commission found more than 7,000 serious incidents of abuse or neglect over the past four years in a sample of seven of the largest providers of disability group homes.15 Other inquiries by the Senate and Victorian Parliament have also been shown evidence of widespread and consistent abuse.16
While neglect and abuse will be a risk in any disability service, research has shown that group homes increase this risk for their residents.
One international study found that community participation results for group-home residents were no better than for people living in nursing homes.17
Some of the highest-risk elements for group-home residents include:
- A lack of choice over key aspects of their home life, such as who they live with, where they live, and the staff who provide support;18
- Isolation and limited contact with people outside the residence;19 Large numbers of staff providing support to residents;20
- A lack of valued interpersonal relationships between residents and staff providing care;21
- A service culture that puts the needs of staff first;22 and
- Violence between residents in group homes.23
Many of these features are endemic to group homes in Australia.
Many group homes effectively operate as ‘closed systems’, where the landlord is also the service provider. This means residents can lose the roof over their heads if they are unhappy with their support and attempt to make changes to it.24
The committee overseeing the the UN Convention on the Rights of Persons with Disabilities has expressed dismay at the group home situation in Australia, recommending a national framework to facilitate their closure.25
The Royal Commission called for major reform in disability housing and support, and a majority of commissioners recommended group homes be phased out over the next 15 years.26
Despite extensive documentation of problems in group homes, there is no nationally consistent data on who is living in them and the prevalence of mistreatment and abuse. And little is known of the quality of support provided, with no commonly adopted quality measures, benchmarking, or performance reporting specific to these settings. As a consequence, Australians are in the dark about what happens behind the group-home door.
What we do know is that the Royal Commission and the NDIS Independent Advisory Council both concluded that ‘while there was significant variation in the quality of group homes, even the best group homes were not that good’.27
1.3 Costs are high and rising fast
Support for people who need intensive housing and living supports is the most costly part of the NDIS, totalling at least $7.7 billion of payments for the six months ending September 2023.28 That’s 37 per cent of total NDIS payments going to about 7 per cent of people in the scheme.29 Despite their small number, people with intensive housing and living supports cost the NDIS more than those without it who are under 18, or with psychosocial disability and developmental delay combined (Figure 1.3).
The way people get support is an important factor in how much it costs. The plan sizes of people with the highest support needs vary significantly depending on whether they have Supported Independent Living funding or not – jumping from $313,000 without it, to $608,000 with it (Figure 1.4).
When people get Supported Independent Living funding, their package size increases dramatically, reflecting the higher costs of supports for people no longer living with their family.
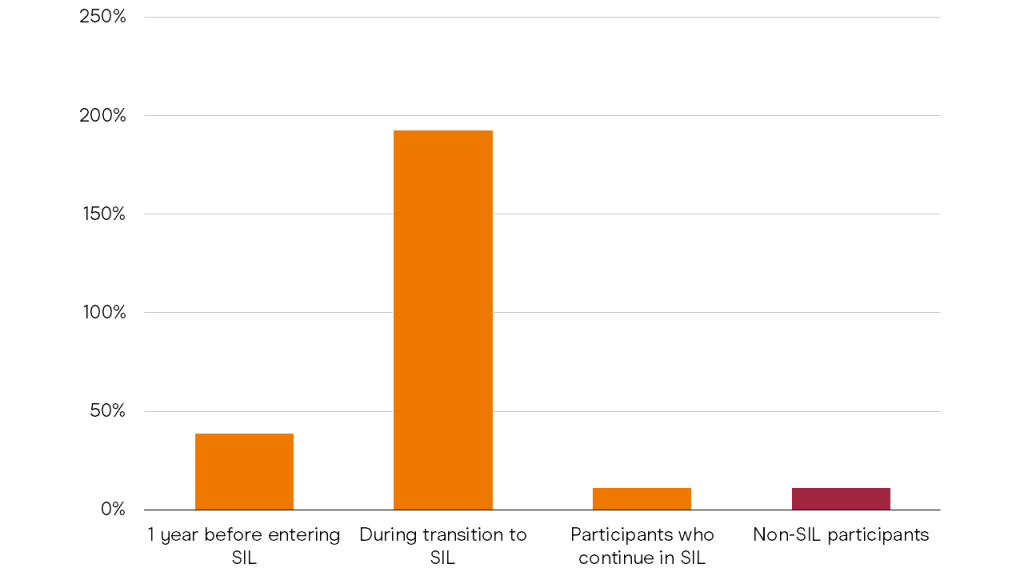
The costs for a typical person who transitions to Supported Independent Living from other NDIS supports, such as when support in the family home becomes unsustainable, will increase by nearly 200 per cent during the year of the transition, compared to annual rises
of 11 per cent for people without this type of funding (Figure 1.5 on page 13).
Finding more efficient ways to provide housing and living support while improving quality and safety is therefore critical to the sustainability of the NDIS.
Figure 1.3: Despite attention on other groups, people receiving intensive living support cost a disproportionate amount to the NDIS
September 2023 for Intensive living support, June 2024 for other groups
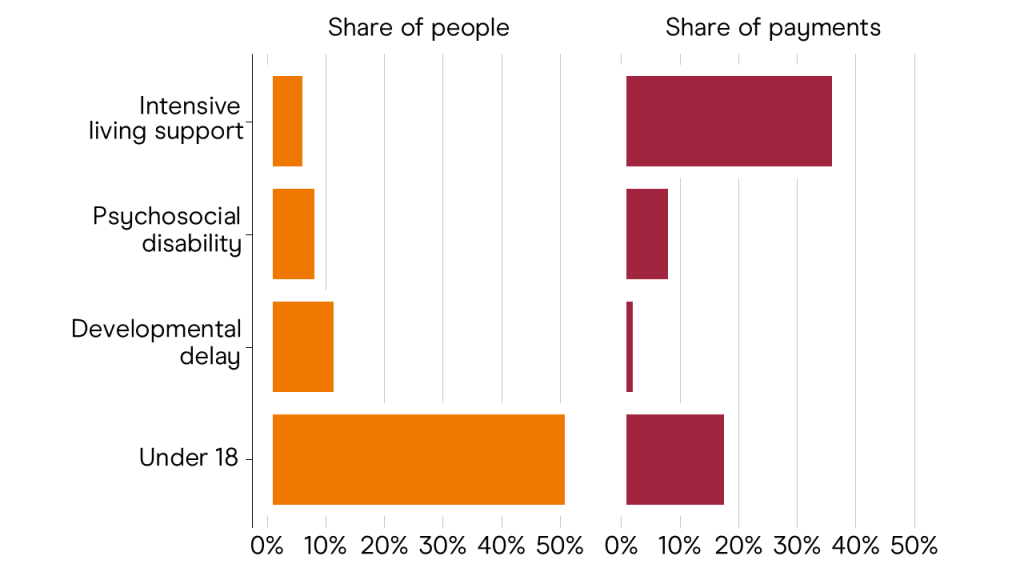
Source: NDIA (2024b).
1.3.1 More people are becoming eligible
Costs are also increasing because more and more people are becoming eligible for housing and living supports each year.
Every year, the NDIS actuary estimates how many people will need Supported Independent Living funding, and in the 2022-23 year there were 3,500 more than expected.30
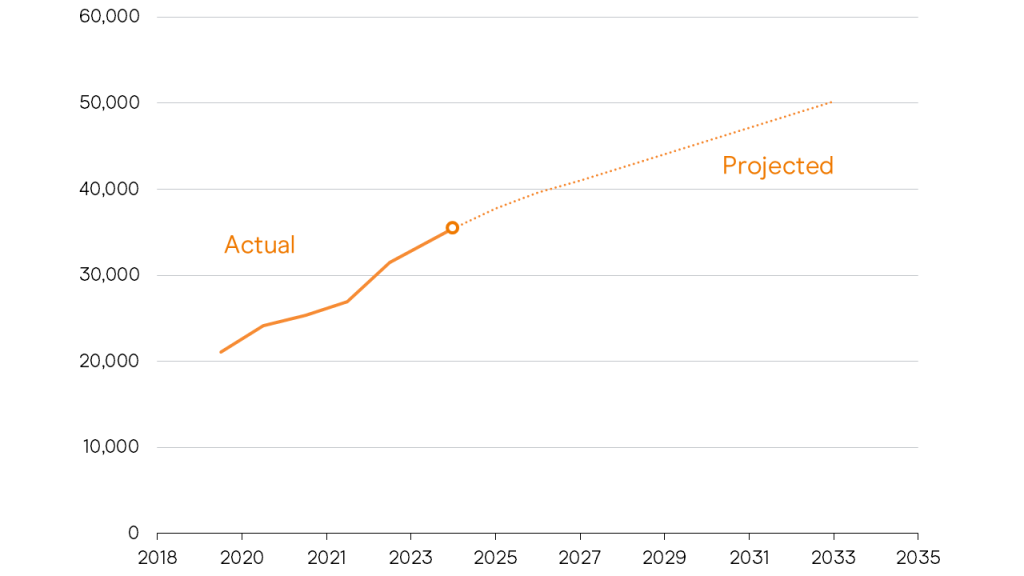
The number of people getting Supported Independent Living funding is projected to further increase steadily as more parents from the Baby Boomer generation grow too old to care for their children and people age within the scheme. The number is projected to be more than 50,000 by 2033, compared to about 34,000 today (Figure 1.6 on page 14).
1.3.2 Providers are struggling
Despite higher numbers needing support and rapidly escalating costs, many providers face challenges balancing their books, with some reporting multiple-year losses.31
Providers have identified rising vacancy rates in older housing stock, shorter resident tenure, and rising labour costs as factors cutting into their revenue.32
Without serious reform, it is likely that providers will continue to struggle to make ends meet, posing further risks to the quality and continuity of support for people with intensive needs.
Figure 1.4: Supported Independent Living funding greatly increases people’s NDIS package size
Median package size by level of function (a measure used by the NDIS to indicate the level of a person’s disability), 2023
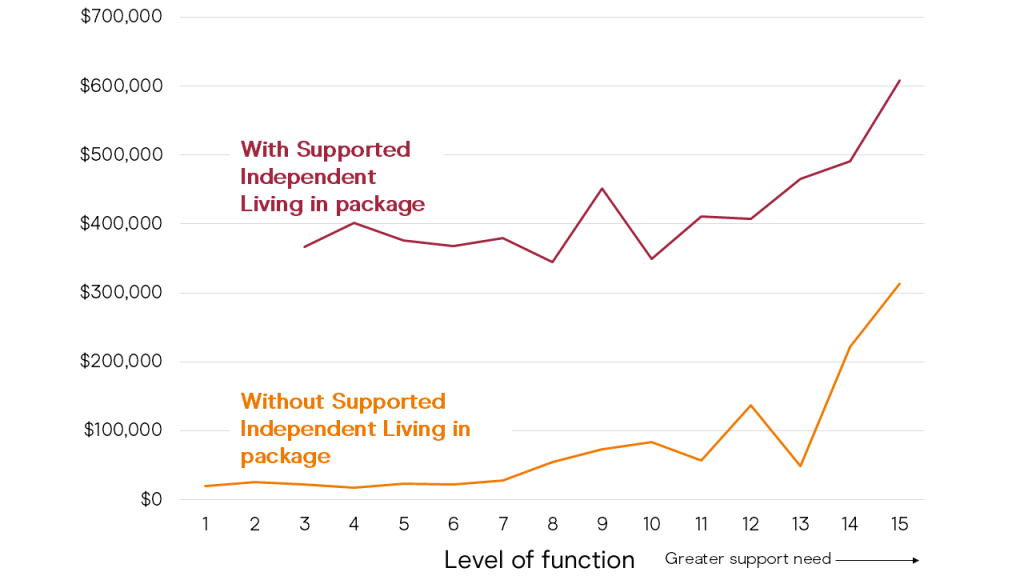
Source: ABS (2023a).
1.4 Money doesn’t always go to the people who need it most
While total costs are through the roof, individual funding decisions are inconsistent and inequitable, with little relationship discernible between funding and need.33
Most people who receive Supported Independent Living funding live in group homes, and these tend to have staffing requirements that don’t relate much to need. For example, a three-person group home will usually be required to have a staff member present 24/7, regardless of how much work there is to do.
As a result, people with different care needs have no difference in package size. Funding only starts to increase for people with extremely high care needs (Figure 1.4 on the previous page).
1.5 The need for change is clear
Recognising the seriousness of the problems facing the NDIS, the Albanese Government commissioned an independent review into the design, operations, and sustainability of the scheme. The review has recommended several relevant reforms:
- More help for families to navigate their way through the system, understand their options, and get the support they need;
- More transparent decision making and budget setting;
- More flexibility for people in how they can use their allocated housing and living funding;
- An expansion in the number of people who can get Specialist Disability Accommodation funding;
- Accelerating the move to ensure all new homes meet a minimum national standard for accessibility;
- Strengthening regulation so all people in group homes and other shared accommodation are safeguarded against violence, abuse, and neglect.
Figure 1.5: Costs rise steeply when people receive Supported Independent Living
Change in size of package from year-to-year
The review also sets the ambition to shift to a system where people ‘always have a say about their living arrangements and the supports they receive, in line with community norms and within the bounds of their allocated budget,’34 but its recommendation that these budgets be pegged to the cost of each person sharing support with two others has left many unsure how this change will be realised.35
The government has committed $468.7 million over five years to help get the NDIS back on track, including $20 million over two years to commence consultation on and design of a new service navigation approach, and a further $129.8 million over two years to consult on other review recommendations, including those relating to housing and living supports.36
1.5.1 Moving away from group homes is possible and desirable
While the recommendations made by the NDIS Review could lead to some improvements, they don’t provide a sufficient roadmap for how to transform group homes and create alternative housing and support options.
And yet, there are tens of thousands of disabled people – some who already have housing and living supports, and some who are yet to need them – who would benefit from this greater choice.
Figure 1.6: The number of people who require Supported Independent Living funding is expected to keep rising
Number of people with Supported Independent Living funding
There are more than 250 large group homes in Australia, sometimes called ‘legacy stock’. These are mini-institutions housing from six to 20 people at a time, removed and isolated from the community.37 These group homes were administratively transferred into the NDIS, but their residents were never offered anything different. Most of these people live in the same conditions now as they had more then a decade ago.
There are also an estimated 17,000 people living at home with a household member over 65 providing unpaid care who will need intensive support at some time in future.38 As their Baby Boomer parents age, increasing numbers of parents will no longer be able to care for their disabled adult children.
Both of these groups of people deserve to have choices about where to live and how to receive support. But without a clear plan, it is unlikely they will see any change.
1.5 Reform efforts so far have faltered
A combination of factors has meant that innovations in NDIS housing39 and support have yet to materialise at scale or crystallise as widely available alternatives to group homes. These factors have included:
- No strategic priority to advance innovation or reduce reliance on institutional support models;
- A lack of funding to trial, evaluate, or spread alternatives to group homes;
- No support or incentives for providers to adjust their business models to offer new things;
- Operational decision making that continues to channel people with intensive needs to group homes due to the perceived necessity of economies of scale in providing their support;
- A lack of active promotion of alternatives by the NDIA;
- A lack of information, advice, and support for disabled people and their families to help them understand their options and coordinate services;
- Policy settings that undermine the financial viability of alternatives, such as denying indexation to innovative arrangements.
We give more detail in Appendix A on why innovative alternatives to group homes have not yet taken hold in the NDIS.
1.7 How the remainder of this report is structured
Chapter 2 identifies alternatives to group homes, and shows that creating a wider range of options could deliver better results for disabled people and greater value for the public purse.
Chapter 3 makes recommendations to transform group homes by transitioning services to share house arrangements that give residents more choice and autonomy over their home life.
And Chapters 4 and 5 set out what else needs to change in the NDIS to make these reforms happen.
Taken together, our proposals are a practical plan to make NDIS housing and support better, safer, and more sustainable.
Chapter 2: Create alternative options
Better living arrangements are possible, even within the NDIS’s budget constraints. Group homes are not the only option, and there are more ways to make supports cost-effective than economy of scale.
And yet, most people who need intensive housing and living supports don’t get the options they need. The current system pushes people into group homes – often the only choice available to disabled people who want or need to leave home. These specialised arrangements are costly and risk segregating people with disability from their community.
Innovative alternatives do exist in pockets around Australia, with people living in neighbouring apartments and sharing a support worker, or on their own with a support worker on-call overnight. But there has been little innovation in how living supports are delivered, and an almost exclusive reliance on paid support workers.
Enabling more people to live in ordinary homes in the community in settings that maximise different kinds of support could improve the lives of people with disability while also increasing safeguards and improving quality – all within the current funding envelope for these supports.
2.1 There are already pockets of innovation across Australia, but they won’t be enough alone
The introduction of the NDIS has spurred some innovation in housing and support options (see Figure 2.1 on the following page for a summary of 12 promising approaches).
Some services rely on people with a disability sharing the same workers, but without living in the same home. This can be most effective where people need only occasional support overnight and are capable of asking for help.
Disabled people in parts of Sydney’s eastern suburbs can call to have a support worker from Spinal Cord Injuries Australia come to their home from 6pm to 5am, with an average 15-minute response time.
This means people who need services overnight (such as a catheter change) can still live independently without paying a support worker to be on site all night.40
If people need more frequent support, some types of Specialist Disability Accommodation enable 5 to 10 people with a disability to live in different apartments in the same building as sole occupancy residents, while sharing support from a single support worker who can
help overnight if there are problems. The support worker typically stays in a separate apartment within the same development.41
The Community Living Initiative in Cairns is a model of housing and living support designed for Aboriginal and Torres Strait Islander people with disability.42 The initiative provides culturally informed support.
A post-occupancy survey indicated improved social and emotional wellbeing for tenants.43
These pockets of innovation are promising; but much more innovation is needed in housing, in the way support is provided, and in the way technology is used. Harnessing these innovations will be key to giving disabled Australians genuine choice over housing and living supports that promote their independence and help make the NDIS sustainable. The remainder of this chapter focuses on the potential of what we call Individualised Living Arrangements.
Figure 2.1: 12 promising examples of innovation that can create alternative options, spanning housing, support, and technology
| Housing | Support | Technology/Remote Services |
|---|---|---|
| KeyRing 10 individuals live in close proximity in the community, comprising nine people with disability and a Community Living Volunteer who lives rent- free in exchange for some support (UK, Vic) | Hosts An adult who needs long-term support is carefully matched with a host, often a family, that provides support, companionship, and a welcoming home life (UK, US, WA) | Occasional and Emergency Service Night call-out service with an average 15-minute response time, enabling people with disability who need services overnight (such as a catheter change) to live independently without a support worker on site (NSW) |
| Community Living Initiative A model of housing and support designed specifically for Aboriginal and Torres Strait Islander people with disability, with support and governance built to create a culturally safe service (Qld) | Home-share A home-sharer lives with a disabled person in their home (rented or owned) and provides support and companionship in exchange for low- cost or free accommodation (Australia, UK, Canada) | Just Roaming Uses sensors to monitor activities in real-time, combined with in-person support from ‘roaming’ support workers (UK) |
| 10+1 10 single-occupancy apartments, integrated in a larger apartment complex, with one additional apartment as a base for support workers who provide onsite shared support 24/7 (Vic) | Good Neighbour Community members are offered reduced rent in exchange for providing informal support to a disabled person living in the neighbourhood, or in the same complex (Canada, WA) | Telecare and Remote Support Uses sensors to enable passive monitoring and check-ins by family or support services, for people with intellectual disability, funded under Medicaid (US) |
| Haven Integrated social housing and support services for people with psychosocial disability, with long-term housing and 24/7 onsite support (Vic) | The Buurtzorg Model Self-organising teams within a neighbourhood, with reduced layers of management, and autonomy to determine the support someone needs to be more self-sufficient in their own home (Netherlands, WA, Qld) | Emergency After-Hours Response Services Overnight telephone support service for non- medical emergencies which can assist with organising in-home support at short notice (Vic) |
2.1.1 The NDIS needs to innovate more with Individualised Living Arrangements
Individualised Living Arrangements (ILAs) are innovative housing and living support arrangements that can give people with disability greater flexibility, independence, and choice. ILAs will typically cost the same as, or less than, a group home, and provide a higher quality of life.
Individualised Living Arrangements differ from group homes in three main ways. They:
- Are integrated into the community as much as possible through the location of housing, living with community members, and building relationships in the local community.
- Use semi-formal and informal support as much as possible, rather than relying solely on formal support.
- Free people with disability from having to share supports.
There are many types of ILAs, including hosts, home-share, co-residents, good neighbour and mentoring, all of which enable people with significant disabilities to live independently in regular homes, with people they choose to live with, with access to the broader community, and often at a lower cost than similar support would cost in group homes.
In Australia and abroad, a growing number of people with disability call Individualised Living Arrangements ‘home’.
Western Australia has pioneered ILAs. Individualised housing and living support has been an option in WA since the 1990s, and today there are multiple approaches tailored to people’s circumstances.
Disabled people in WA have taken up Individualised Living Options at a much greater rate than disabled people in other parts of the country (Figure 2.2 on the next page).
In British Columbia in Canada, Home Sharing is the main type of residential support for people with intellectual and developmental disability funded by the provincial government, overtaking group homes as the most common choice of living arrangement.44 Large institutions were phased out entirely in the late 1990s, and today, more than 4,000 people live in home sharing arrangements – in a province that is only a quarter the size of Australia.45
In the UK, just under 10,000 people were being supported in Shared Lives arrangements similar to ILAs in 2022-23. People with disability either lives full-time with their Shared Lives carer, or they visit as needed. Quality and safety tend to be high in these arrangements: 97 per cent of Shared Lives arrangements in England have been rated as ‘good’ or ‘outstanding’.46 The UK government awarded Shared Lives England funding in October 2023 to expand the program, as part of a fund to increase innovation in adult social care.47
Individualised living arrangements in the US show promising results, with many states having host family arrangements. Of Americans with disability who were receiving residential services and living out of the family home in 2012, nearly 8.6 per cent were living in a host/foster family arrangement (including children in foster care).48
While every Individualised Living Arrangement differs depending on the person’s needs and circumstances, we focus on two main types of arrangement in this report because we think they have the greatest potential for widespread use: hosts and home-share.
2.1.2 Hosts
A host arrangement is where an adult with NDIS funding lives with a ‘host family’ or ‘host flatmate’, who is not related to them, in the host’s home, becoming part of the household.
The arrangement is very similar to how foster care works in Australia today. A host might be a couple or an individual, and they provide semi- formal support while going about their everyday activities.
The host might help with emotional support, companionship, cooking, cleaning, and other household tasks. In exchange, they receive a subsidy for their expenses. Hosts can also receive rental payments directly from the person living in their home.
To facilitate these arrangements, a service agreement is developed detailing the roles and responsibilities of the host, the person receiving support, and the provider facilitating the arrangement. Hosts typically support a single person in their home, except in extraordinary circumstances, such as when two siblings with a disability want to live together.
In addition to support provided by the host, people with disability can also receive other kinds of support, such as informal support from family, friends, or neighbours, or regular shifts from paid support workers who provide drop-in or on-call assistance.
Figure 2.2: Individualised Living Options are most popular in WA, where innovation has thrived
Number of people in the NDIS, per thousand, with Individualised Living Option funding, December 2023
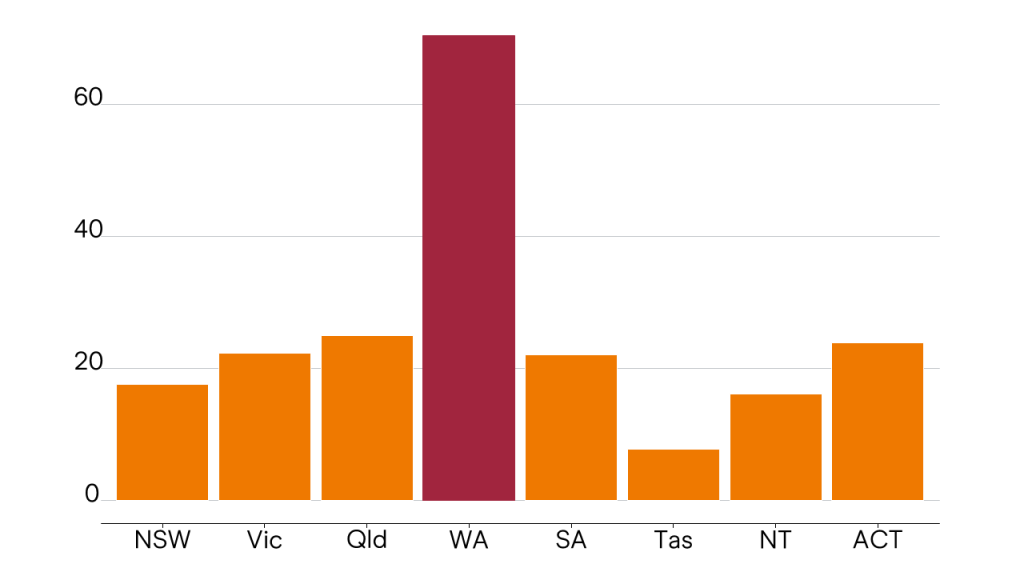
Source: Grattan analysis of NDIA data.
Box 1: Anja’s host family arrangement
Anja* is 23 and has an intellectual disability and needs help with household tasks and planning her days. Anja lives with Sarah and David in a host family arrangement set up by a registered provider and her family.
David works full time and Sarah works part time. Sarah and David do the cooking, cleaning, laundry, and home maintenance. Sarah is helping Anja learn to make breakfast for herself.
During the week, Sarah, David, and Anja usually eat dinner together. On weekends, Anja and Sarah go out to run errands or meet people. Sarah and David are at home overnight if Anja needs help during the night, although this doesn’t happen often. Sarah and David like to host barbeques in their backyard with friends once a month, and Anja is getting to know them all. Anja volunteers two mornings a week at a local op shop and likes to visit her family on Sundays.
Anja’s NDIS plan means she can get four hours per day of one-to-one community activity time with support workers that she has hired, which she uses for personal shopping, going to the gym, and joining community activities or meeting friends.
Being independent, out of her parents’ home, and having the freedom to be flexible with her time are some of the reasons Anja likes being in her host family arrangement.
For four weeks a year, Anja, Sarah, and David take a break from the host arrangement and Anja uses her short-term accommodation (STA) budget to stay elsewhere, perhaps with her family or with friends.
Sarah and David receive a subsidy for the expense of Anja living with them at $65,000 per year. The provider is responsible for ensuring the arrangement is working for Anja and Sarah and David, and will meet regularly with each of them, oversee the direct-care staff, and communicate regularly with Anja’s family.
*This is a fictional case study, for illustrative purposes.
2.1.3 Home-share
In this type of arrangement, an adult with disability lives in their own home (owned or rented) with a housemate who provides in-kind support in exchange for a subsidy for expenses, which often partially or wholly covers their rent.
Typically, where a housemate only receives free or reduced rent, they will provide less support than in a host family arrangement (up to 12 hours per week for a flatmate on top of passive overnight support), though this is open to negotiation.
As with host families, the preferences and needs of the person with disability and the housemate are laid out in a service agreement signed by all parties. Home sharers should enter into an agreement with only one person with disability, except in extraordinary circumstances, such as siblings who want to live together.
And as with a host arrangement, people with disability receive other kinds of support, including from paid support workers or through informal support, in addition to support from their home-sharer.
Box 2: Steven’s home-share arrangement
Steven* is 26 and has autism and needs help with problem solving, managing unfamiliar situations, and verbal communica- tion. He rents an apartment in Sydney with his flatmate, Jack. They’ve been living together for nearly a year, in a home-share arrangement that a registered provider helped them establish.
Steven works part time at a local supermarket, and Jack works full time as a landscaper. Steven usually works in the morning, and then goes out into the community with his support worker in the afternoon. Steven gets four hours per day of one-to-one support worker time with a team of support workers he has chosen.
Jack makes dinner for them both and Steven helps to stack the dishwasher and clean up. The routine that Jack and Steven have created helps Steven manage his anxiety.
Jack is home most nights in case Steven needs help, and when he’s not home, Steven can call his mum and dad or the overnight and emergency service if he needs help.
On the weekends, Jack and Steven like to go to the pub to watch the footy, and sometimes their friends join them.
Steven’s home and living package covers Jack’s rent as an acknowledgement of the household assistance, emotional support, companionship, and any emergency support required when Jack is home.
Steven wants to be independent, and he’s hoping to increase his work hours this year, either at the supermarket or at another job, or to study at TAFE.
*This is a fictional case study, for illustrative purposes.
2.2 Individualised Living Arrangements can be cost-effective
Individualised Living Arrangements can be cheaper than group homes because they tap into semi-formal support, instead of relying solely on rostered, paid support workers.
There are three kinds of support available to people with disability:
- Informal support is the kind of support provided by friends and family on a voluntary basis;
- Formal support is provided by professional support workers who are usually paid by the hour; and
- Semi-formal supports, which sit in the middle. These are services provided by people who want to provide support, but need to be subsidised for the costs associated with doing so.49
Semi-formal supports tend to be integrated into the life of the person providing support, and do not require the payment of an hourly salary.
While these arrangements can require more administration to set up, they tend to be less expensive than formal supports provided by workers paid by the hour.
Because the NDIS currently draws on only formal or informal support, people with disability and their families are frequently left with an ‘all or nothing’ approach: either a professional, paid-by-the-hour worker provides support, or it’s volunteered by family or friends.
The ‘all or nothing’ approach also means that some people are getting support they don’t need. In group homes, for example, residents share round-the-clock assistance from a support worker, at ratios ranging from one-to-three (using one-third of a support worker’s time) to one-to-one or higher in the most extreme cases.
The need for support is usually not exactly matched to the ratio of staffing provided. If a person with disability living in a group home needs support intermittently and unpredictably (for example, frequently at some times of the year and not others, or once a week on average but on different nights each week), then in practice it costs a similar amount to staff a support worker for this person as it does for a person who needs support every night – a worker is paid for an overnight shift whether the person needs their help or not.
Semi-formal support is a much more cost-effective way of giving people with disability the support they need, because it avoids the waste associated with a paid support worker whose labour is demanded only occasionally and yet supplied constantly. The semi-formal supporter lives their everyday life, and is available in case the person with disability needs them.
By adding semi-formal supports to the mix, Individualised Living Arrangements can be cheaper than group homes, which rely solely on formal support.
Grattan Institute analysis of data from Individualised Living Arrangement providers in Australia indicates that, on average, ILAs cost about
$183,000 per person per year, or about $45,000 less than a group home with supports shared at a ratio of one-to-three, which is the benchmark recommended by the Independent Review of the NDIS (Figure 2.3 on the following page).
Although a benchmark can help the National Disability Insurance Agency to centrally plan spending, a single one-to-three benchmark for housing and living support is unnecessarily restrictive. In Chapter 4 on page 36, we propose three funding bands that would cover the majority of people who need intensive housing and living support.
Anyone can call an Individualised Living Arrangement ‘home’, with the right match between the person with disability and their host or housemate. As people with disability transition away from group homes, it is likely that people who need passive overnight support will be the first to take up more innovative alternatives. Those who need active overnight support may need a support worker to stay in their home overnight. Even with this additional cost, it is possible that Individualised Living Arrangements could be more cost-effective than receiving round-the-clock formal support at a ratio of one-to-two or one-to-one (see Appendix B).
Figure 2.3: Individualised Living Arrangements cost less than group homes
Per person yearly cost of housing and living arrangements, 2024-25 dollars
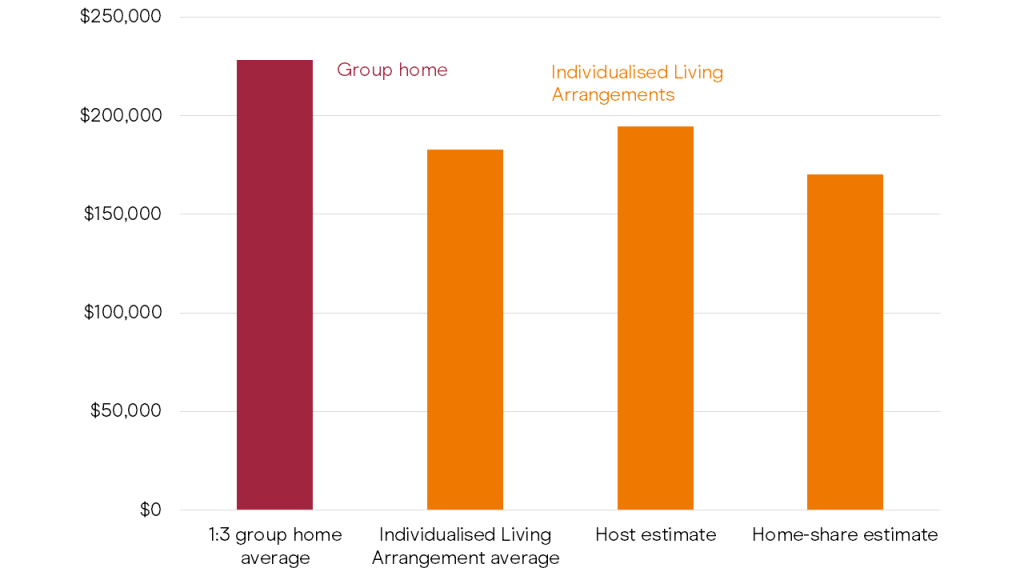
Sources: NDIS Review (2023); Grattan analysis of unpublished provider data (2024).
Box 3: The flexibility in Individualised Living Arrangements creates savings
Sharing supports in a group home creates an economy of scale – three people can share one support worker, rather than living separately and needing one support worker each.
But sharing support workers also creates constraints. If one person goes to stay with their family for the weekend, the other two people still need rostered support workers. The cost is the same, even though fewer people are receiving a service. This means there are no savings to the NDIS from the person spending time with family and friends, rather than with support workers.
To save money, all three people with disability would need to stay with their families over the same weekend – a difficult coordination task.
Individualised Living Arrangements are more flexible than group homes. Informal and semi-formal supports are built into the service, instead of disabled people having to almost always rely on formal support.
2.2.1 Host arrangements can be cost-effective
Host arrangements can be cheaper than group homes, without the requirement for supports to be shared.
This is shown in Figure 2.4 on the following page where we compare costs against the NDIS Review benchmark of intensive living support funding set at one support worker for every three eligible people.50 The cost of providing living support for a resident in a one-to-three group home, with someone present overnight, is about $228,000 per person, per year (Figure 2.3 on the previous page).
A typical host arrangement might involve the person with disability receiving four hours of formal, paid support per day, costing about $109,000 per year. This support enables the host to work or engage in other social activities. People might use this time in different ways: some might prefer one or two days per week when they are not providing support; others might like help with particularly challenging parts of the daily routine.
Host agreements would also provide four weeks of short-term accommodation so that people with disability and their hosts can take a break, typical of NDIS arrangements where care is provided by non-professional workers. This would cost about $26,000 per year.
And providers would require some compensation (on top of the usual administration fees which are built into the price guide). A fee of 21.65 per cent for operational overheads, 12 per cent for corporate overheads, and a 2 per cent margin applied to the host subsidy to cover support with ongoing maintenance, review, and adjustment of the service, would cost about $25,000 per year.51
This would still leave more than $67,000 available to compensate hosts. It’s unlikely that hosts would require the full $67,000, and there is therefore considerable room to enable system savings.
Figure 2.4: Host arrangements can save money
Cost per year of innovative arrangements, 2024-25 dollars
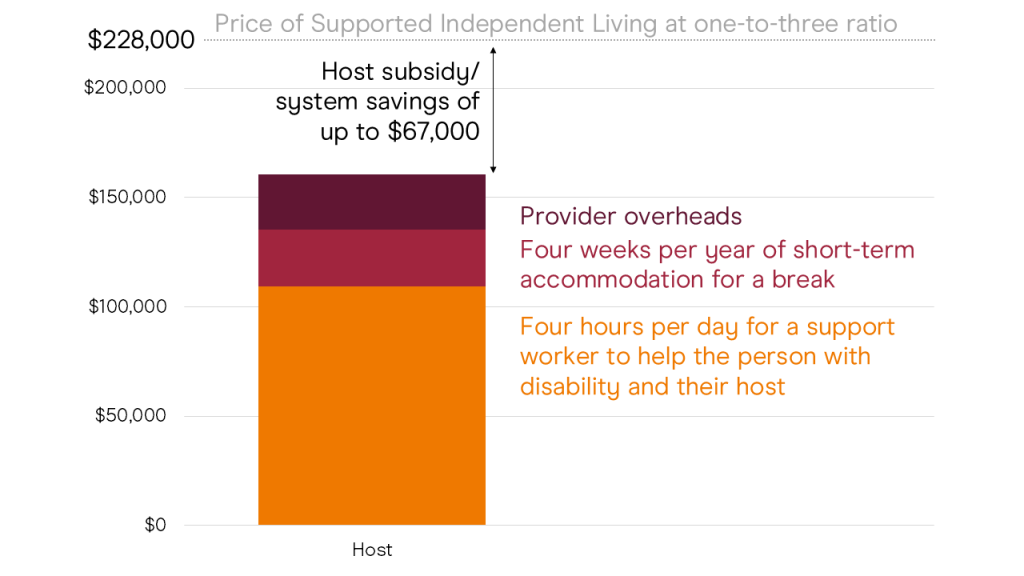
Figure 2.5: Home-share arrangements can save money
Cost per year of innovative arrangements, 2024-25 dollars
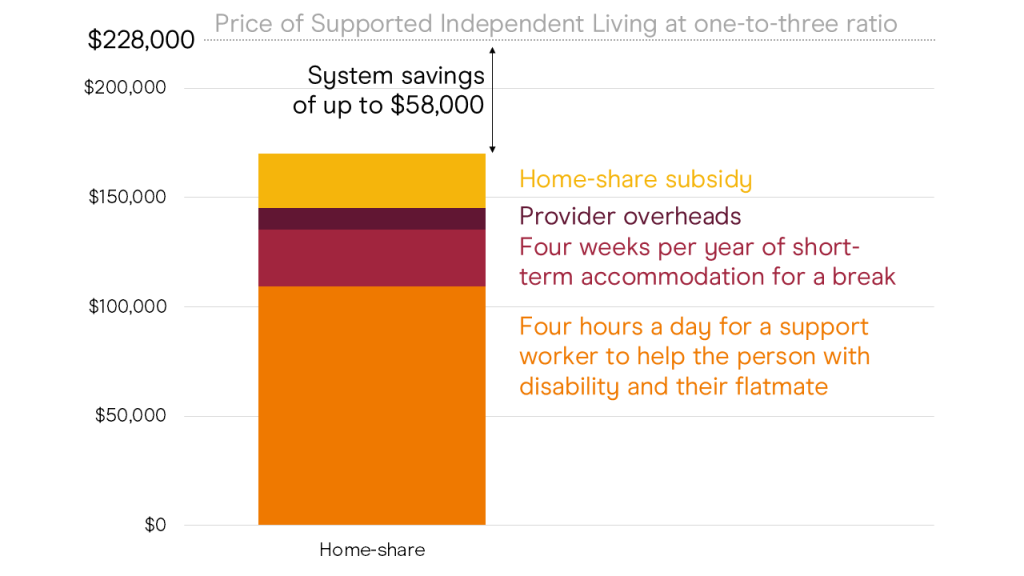
Source: Grattan analysis of NDIA data.
2.2.2 Home-share can be cost effective
The usually lower support requirements of people in home-share arrangements provide even greater opportunity for savings.
We recommend similar short-term accommodation and daily support for disabled people in home-share arrangements as in host arrangements. And providers compensation of 21.65 per cent for operational overheads, 12 per cent for corporate overheads, and a 2 per cent margin applied to the flatmate’s subsidy to cover support with ongoing maintenance, review, and adjustment of the service, would cost about $9,700 per year.
A subsidy of $25,000 for the flatmate providing support would still enable a system saving of $58,000 per year, as shown in Figure 2.5 on the preceding page, though this saving would be lower in instances where the agreed level of support is higher, attracting a higher subsidy.52
2.3 Individualised Living Arrangements promote genuine choice for people with disability
Individualised Living Arrangements provide another option for people with a disability, away from the old system of group homes.
Although the NDIS seeks to promote choice and control for people with disability, merely promoting choice without creating options is a meaningless exercise. Currently, people with intensive needs often have few choices when it comes to their housing and living supports;
which house they live in, who their housemates are, who provides them with support, who helps them get in and out of the shower, or what they eat and when.
Stimulating growth in Individualised Living Arrangements promotes choice at two levels, first by expanding the number of service options and providers available to people with intensive support needs,53 and second by improving the choices they can make within the service, over where they live and who they live with, as well as who provides support and how.
These kinds of choices are a central focus of the planning and design of Individualised Living Arrangements.54
This matters because research indicates that people with disability who choose their services, supports, and who they live with, tend to have better quality of life.55
Choosing who provides your services matters too. People who need intensive living supports are in frequent, close contact with their support workers. If you need help getting in and out of the shower or bed, getting dressed, or using the bathroom, who helps you is a decision you want control over. The way in which support is provided is just as important as what is provided.56
For disabled people living in rural or remote areas, having the option to live with a host, or rent a property in the private market in a home-share arrangement, could be the difference between living in your community, and having to move to get the services you need.
2.4 Safeguarding Individualised Living Arrangements
Individualised Living Arrangements with appropriate safeguards also offer the potential to improve the safety of people living with disability.
ILAs tend to have an explicit focus on building people’s independence, and expanding their social networks. Building these natural networks of support can be a crucial factor in ensuring participation in the community and keeping people safe.57
However, there are clearly risks to a person with disability living with another family in their home, or with flatmates. The risk of exploitation58 means that the design of ILAs is important, particularly to ensure that there are a range of supports in the package and the disabled person has regular contact with multiple people, rather than relying solely on their host or flatmate.
Individualised Living Arrangements should usually be overseen by a registered provider who can step in when needed. There should also be external oversight and check-ins, to make sure the person with disability is safe and happy.
There should always be formal support in host arrangements, as well as informal support where possible, so that the person with disability is receiving support from a variety of people and not only the host. The registered provider overseeing the host or home-share arrangement can hire staff directly, because they do not own the property in Individualised Living Arrangements.
Hosts and flatmates are not employees, so there is no need for them to register. However, the provider managing the arrangement should be registered, and they must have up-to-date information about hosts or flatmates. Registered providers should require hosts and flatmates to complete a worker screening check.
If the person with disability is self-directing their supports, then they should register themselves so that their support providers, including hosts or flatmates as semi-formal supports, are visible, as recommended by the NDIS Provider and Worker Registration Taskforce.59 Capacity-building for people who are self-directing their supports should prioritise those with Individualised Living Arrangements.60
Hosts and flatmates should not have power over disabled people’s plan funding, or any other role in their plans. Semi-formal supporters need explicit training that should be outlined in the practice standards for Individualised Living Arrangements, and access to capacity-building support (see Chapter 4).
2.5 Three policy settings to enable Individualised Living Arrangements
So far in this chapter, we’ve shown that creating alternative options for people with intensive housing and living support needs is possible, desirable, and can be cost-effective. Three changes to current policy settings would ensure these options are more widely available to people.
2.5.1 Make hosts and housemates volunteers, not employees
The types of Individualised Living Arrangements we have described are possible under current legislation, so long as specific rules are applied.61
Most importantly, the role of hosts and housemates (and any other semi-formal supporters that might form part of a person’s ILA) must be established as volunteers, not employees. This should be clearly reflected in service agreements.
In these roles, hosts and housemates receive a subsidy for expenses associated with a person with disability living with them. These expenses cannot include items that the NDIS does not cover, such as food, utilities, or the person with disability’s rent (which typically come out of the person’s Disability Support Pension and Commonwealth Rent Assistance).
Expenses might include those associated with the disabled person staying connected to the community, maintaining or building relationships, travel, and more. Within these parameters, subsidies are not subject to income tax, and are excluded from social security income calculations.
We estimate that the subsidy would be similar to the foster care system, with two differences; firstly, foster carers are reimbursed for everyday living expenses, while hosts are not, and secondly, the proposed subsidy acknowledges that people with disability face increased living costs on account of their disability.62
Therefore, we estimate that hosts could be subsidised between $50,000 and $80,000 per year, pegged to the consumer price index and dependent on the costs the host incurs.63
The Agency should produce guidance about the rules for providers and people interested in establishing an Individualised Living Arrangement, so that they are implemented faithfully.
2.5.2 Establish a rental payment to encourage innovation
Transitioning away from group homes and into more innovative options will not succeed if people in the program cannot afford rent. And unstable housing on the private rental market will make it challenging for people in the program to establish long-running care arrangements, essential to any innovative arrangement’s success.
To increase stability for people in innovative housing arrangements, we recommend that the NDIA provide a targeted rental payment to people with intensive living support needs as an alternative to group homes. We outline the details of this payment in Section 3.3 on page 34.
2.5.3 Allow people to keep unspent funds to spend on other services
Based on our analysis, Individualised Living Arrangements often will cost less than group homes and other arrangements that use only formal support. Some people may want to take up more expensive options, because they think the higher price means greater quality, or that the NDIA will take away their funds if they don’t spend every cent. This thinking might lead people to make choices that aren’t in their best interests (or in the best interests of taxpayers).
As an incentive to take up less expensive Individualised Living Arrangements, people in the NDIS should be allowed to keep unspent funds from their home and living budget for an agreed time limit (for example, up to a year). Allowing people with disability to keep unspent funds takes the pressure off them to spend as much as they can, and better aligns their interests with those of the taxpayer. If people with disability do not spend all of these excess funds, there are potential savings to the NDIS and in turn, taxpayers.
People should be able to transfer excess funds from their home and living budget into their general budget to use on other services, such as therapies, capacity building, or community participation. If their home and living supports cost consistently less than the projected cost, the NDIA should consider shifting down their home and living budget in increments, so long as the person’s circumstances have not changed. If home and living budgets are consistently lower, then the NDIA should adjust plan funding benchmarks (see Chapter 4).
Chapter 3: Reform the existing system
Even as more people take the opportunity to move away from group homes, there will still be some who choose to live together and share support. Reform is needed across the system so that the NDIS can fulfil its duty to every person with intensive housing and support needs, regardless of their living arrangement.
Where disabled people make the choice to live with other people who have a disability, it should be in an environment where they retain control over how they live their lives. People with intensive support needs should be able to choose who they live with, who provides their support, and how. The rhythm of their day should be a choice, not something dictated by government or service providers.
These changes should be rolled out as soon as possible to ensure that institutional care does not continue.
The transition away from the institutional-style bricks and mortar of some group homes will take longer. These homes should be replaced over the next 15 years.
3.1 From group homes to share houses
Group homes were favoured when disability care was de- institutionalised, because multiple co-residents enabled providers to share support worker time. But the more people who live in a given house, the more difficult it is to create a home-like environment. The largest group homes, sometimes called ‘legacy stock’, can have six or more residents and are particularly common in Victoria.64
But the presence of group homes in disability care is not inevitable. Western Australia for instance, has pioneered alternative arrange- ments, meaning fewer people need to live in group homes (Section 2.1.1 on page 18).
The Disability Royal Commission called for group homes to be phased out within 15 years, due to poor safety and quality, namely:
- high rates of violence, abuse, neglect, and exploitation in group homes;
- the tendency for residents to be segregated from the community, spending much of their time with paid staff rather than friends, family, and community members.65
Group homes in their current form clearly need to change, but like many Australians who live with their peers in share houses, some disabled people will probably always choose to live with other people with disability. Some people report increased loneliness after moving from group homes to live by themselves, and there is nothing inherently wrong with people deciding they would rather live with other people.66
The NDIS needs a practical plan to enable people with disability to live with other disabled people while maintaining control of their daily life. But to achieve choice within shared living, there needs to be a re-imagining of what a home-like environment is, rather than merely tinkering with the number of people in a house.
The NDIS Review grappled with the trade-off between economic efficiency and providing a home-like environment and recommended a benchmark ratio of one support worker for every three supported residents.67 Some advocated to the review for expanded one-to-one funding of support workers,68 but this would be financially impractical for the scheme.
Economy of scale is not the only way to provide cost-effective support, as Chapter 2 shows. However, it can help to reduce cost where people use only formal support. Costs increase dramatically as the number of residents in a group home falls (Figure 3.1). One-to-one care is
$419,000 more expensive per year per resident than one-to-three care. If that extra money was spent for every person eligible for Supported Independent Living funding, it could cost the scheme up to $14 billion extra per year.
Better still, a growing feature of share-houses could be sharing both formal and semi-formal support. Combining the economy of scale from sharing support workers, with semi-formal support from a housemate, would be a cost-effective way to run share-houses in the future.
The most important difference between a group home and a share house is the level of choice and agency that people have over their day-to-day lives.
Residents should be able to control who they live with, who looks after them, and how. Changing the power-dynamic between providers and residents requires changes to the layout of group homes, the way decisions are made, and how those decisions are enforced.
Many of these changes can be achieved by improving the way support is provided by staff, but some improvements require other structural changes to the way services and residents interact.
Figure 3.1: Shared supports are much cheaper than one-to-one support
Yearly cost for each person with a Supported Independent Living plan, 2024- 25 dollars
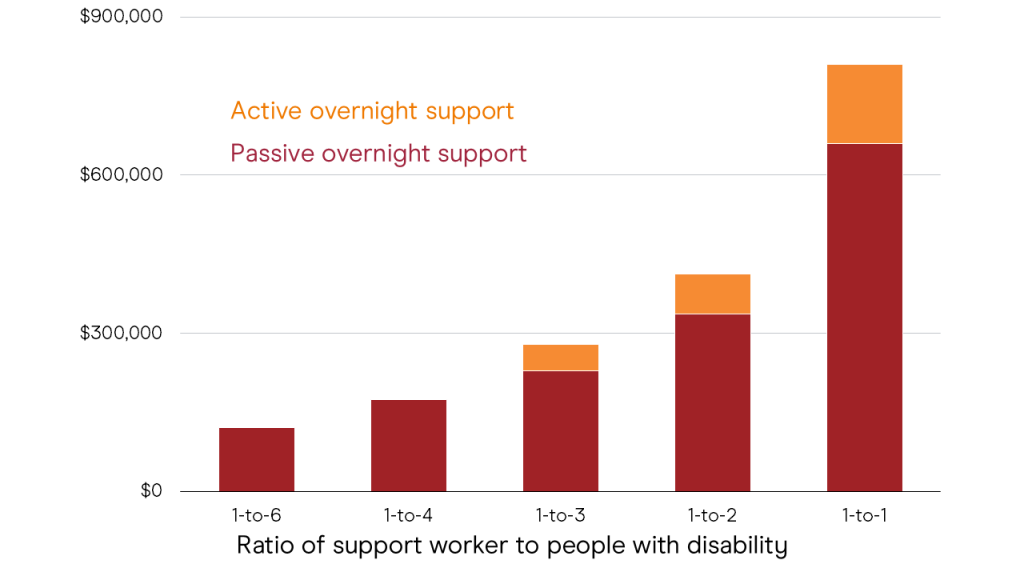
Source: NDIS Review (2023a, p. 548).
3.1.1 Providers need to deliver ‘Active Support’
The biggest factor in determining the quality of supports in shared accommodation is the quality of the staff and organisational supports.69 A prominent way of describing high-quality care is ‘Active Support’, which has been shown to increase engagement in activities for residents in shared accommodation.70 Active Support involves:
- Workers using opportunity to engage with the people they support.
- Workers providing ‘graded assistance’ – just enough so that the person is supported and can develop their own skills.
- Maximising residents’ choice and control.
- Support being provided in frequent, short periods of engagement, to maximise concentration and opportunities for success.
Active Support can be measured in an organisation through surveys that rank support-worker and management adherence to practices that maximise residents’ quality of life. Active Support works best when
the leadership and culture of the organisation continually reinforce it through training and rewarding good practice.71
Training resources developed by people with disability themselves which effectively communicate their needs and preferences to support workers can also improve the way support is provided.72
3.1.2 Residents should make collective decisions about how the household is run
Residents need to have more control over how decisions are made that affect their lives. Resident-led governance means giving share-house residents control over who lives in the house, who the workers are, and the everyday rhythms of the house such as meal-times and outings.
Some residents of group homes have already achieved greater control through resident-led governance, but this is usually only possible with the help of family members who advocate on behalf of their loved ones.73
The NDIS Review mentions Supportive Independent Living Co-operatives, where friends and family of group-home residents employ a ‘housing operator’ that performs all the roles of a registered provider, but with clear lines of governance with the family at the top.74
Another innovative arrangement for resident-led governance is the concept of micro-boards, where members of the community including family and others form a formal support network around a person with a disability.75
While these innovations show promise, residents without family to advocate for them too often end up living their day-to-day lives at the convenience of service providers rather than according to their preferences.
The NDIS Review outlined a series of reforms to overcome this problem, starting with a recommendation to create a new role of shared support facilitators who would act as an intermediary between service providers and residents to advocate for residents’ choices.76
In Chapter 4 on page 36 we advocate for the new role of local housing and living support navigators. One of the functions of this role would be to connect share-house residents with a range of other supports, including support for decision making, micro-boards, advocacy or other capacity building supports, many of which we recommend are directly commissioned by the NDIA.
By employing local navigators who have better knowledge of other options in the local area, the NDIS could also increase the chances that people who are not happy with their current housing situation can find either new housemates and/or a new home.
We don’t think it makes sense for there to be a separate role in the system solely focused on shared support facilitation. It is better for navigators to work with the disabled people they support and connect them to the other supports they need to have control over decisions in the home, all the way from package creation to household mediation and moving house when needed.
3.1.3 Make service agreements enforceable
If disabled people are going to have more control over how care is delivered in shared accommodation, the NDIA needs to help facilitate better agreements between providers and share-house residents.
Currently, the NDIA recommends that all service providers and people they support draft their own service agreements which set out the terms agreed between them. These agreements typically include broad motherhood statements about how all people using the service should be treated with respect, but do not include enough detail to enable residents to negotiate how they spend their everyday lives.
Service agreements should instead be mandatory and include detailed information about how the person with a disability wants to live their life. It should include information about the daily rhythm of the household, as well as how new workers and housemates will be chosen, inducted, or dismissed. The NDIA should provide a standard template to facilitate discussions between disabled people and providers.
These agreements also need to be easily enforceable. Currently, people on the NDIS are directed towards the consumer law regulator to deal with any disputes that might occur as a result of contract disagreements.77 But this regulator is not properly situated to mediate household disputes.
The NDIS Quality and Safeguards Commission should provide a mediation service to facilitate agreement where providers or people using their services feel their service agreement is not being upheld.
After a grace period of 18 months, the new service agreements should be a requirement of all NDIS housing and living support provider registrations.
3.1.4 Separate living and housing supports
For many people who live in group homes, their house and support is currently provided by the same organisation. Real choice in housing and support can’t be achieved where the provider of housing is also the provider of living support. This can mean people’s home is at risk if they want to change who provides support. Consequently, both the Disability Royal Commission and the NDIS Review recommended the separation of housing and living support.78
Separating the provision of housing and living supports would give people more freedom to choose their support workers.
As group homes are phased out, and more people move into other housing, the NDIS should mandate that by default, all new housing is provided by a different operator to the one providing living supports.
Over time, existing operators that provide integrated services should be phased out. After a grace period of 18 months, all providers should need as part of their registration process to demonstrate that they have moved away from integrated living and housing supports.
These operators should be given time to make the transition, because they might choose to exit the market if the transition is too sudden.
For some services, integration might make sense, for instance where a short-term service is introducing positive behaviour support to address behaviours of concern, or in the case of host arrangements where hosts provide some living support and housing for the person with disability, alongside formal support from workers. These services should be able to apply for an exemption to the requirement of separation between housing and living. These integrated arrangements should be reviewed every five years, or earlier if requested by residents, to manage conflicts of interest, ensure that a high-quality service is being provided, and check that intended results for residents are being achieved.
3.1.5 Fund providers so there is time for vacancies
Just like people who live in any share house, people with disability need to be happy with the people they live with. But the job of finding the right person to move in with can be a lot more challenging for people with intensive support needs.
Where the intention is to share supports, there are only a small number of people eligible for these services, and the average tenure of people in group homes or specialist housing is much longer than in the typical rental market. As a result, finding the right person to fill a vacancy can take time.
Specialist Disability Accommodation rules reflect the challenges that can be faced finding a new tenant, but there is no such help for providers of intensive in-home supports.
An SDA provider will get paid for between 60 and 90 days where there is a single vacancy in a multi-person dwelling.79 But only four weeks leeway is granted to support providers when there is a vacancy in
their service roster.80 As a result, people in group homes are either not properly consulted on their new housemate or are pressured to accept a new resident who is not the best fit.
The NDIS should fund both SDA and in-home support providers in multi-person living situations for vacancies for up to 60 days, to enable the remaining residents to find the right housemate to join their share house. Service agreements should set out protocols for how residents can lead decision making when filling a vacancy in their home.
After 60 days, providers should be able to apply for extra funding and more time, provided they can demonstrate that significant effort has been made to find a new housemate, for instance by interviewing potential candidates.
These vacancy payments would add some costs to share-house administration, but these costs should be offset by greater stability in housing arrangements, fewer disagreements between residents, and fewer complaints and reportable incidents.
3.2 End legacy stock within 5 years
As more people transition away from group homes, there needs to be a timeline to completely close any houses that have an institutional-like architecture. While some group-home stock may be able to provide share-house like environments, other homes (particularly legacy stock) are far too institutional to make the switch.
As a first step, no new institutional-like buildings should be built. But replacing existing stock will take time. Given only 825 new-build Specialist Disability Accommodation dwellings were enrolled in 2021-22, Australia’s unsuitable group homes cannot be replaced overnight. For legacy stock (with 6 bedrooms or more) a timeline of 5 years is enough to transition to more suitable dwellings. For group homes with 4 and 5 bedrooms a timeline of 15 years is more than enough to ensure housing demand is met for existing population growth, while transitioning to more suitable accommodation. This timeline also recognises the challenges faced by existing residents who may not want to move home.
By 2040, no Australian should be living in a group home unless they have been given reasonable opportunities to choose to leave their existing house and chosen not to do so.
3.3 Don’t use Specialist Disability Accommodation housing to entrench the group-home system
When people with intensive needs require highly specialised housing, they become eligible for Specialist Disability Accommodation funding to account for the extra cost of providing their home. People that entered the NDIS in group homes previously run by the States all automatically qualify for SDA as well.
Over the coming decade, a significant expansion of new SDA housing is expected as more people are transferred out of ageing housing stock.
But not everybody with intensive in-home support needs currently qualifies for SDA. Some people are not eligible because they don’t require a highly specialised home.
Finding an appropriate place to live is difficult for all Australian renters. Rents are up nearly 12 per cent since the start of 2022. They rose 7.3 per cent in the last year alone. To make rent more affordable, Grattan has previously recommended at least a 40 per cent increase in Commonwealth Rent Assistance.81
But people who receive intensive living support face extra difficulties not faced by other renters in the private rental market.
Many of these people are living in non-SDA group homes, boarding houses, or Supported Residential Services. The NDIS Review heard that many of these people are currently targeted by unscrupulous provider-landlords because of their large support packages.82 The NDIA has no visibility of these arrangements, and the regulator is oblivious to their quality.
Rent is not currently paid by the NDIS, and this group’s only way to pay rent is typically with the Disability Support Pension and Commonwealth Rent Assistance. And moving house can be particularly socially dislocating for people who need intense housing and living support.
If they need to move to an area where there is cheaper rent, doing so will often result in the loss of the informal support of family and friends, and the gap needs to be made up with much more expensive formal supports.
Where people with intensive support needs are not eligible for one of the current Specialist Disability Accommodation categories, or wish to move away from their group home, they should instead get a housing payment that can be used in the private rental market.83 This could be spent on a new lease, or be paid to the current housing provider where people are content with their living situation.
This payment would encourage longer rental agreements and reduce the geographical dislocation that can happen when rents go up in a given city.
The rental payment should be set at a level which:
- Ensures that a person would not need to spend more than 25 per cent of their Disability Support Pension plus 100 per cent of their Commonwealth Rent Assistance to pay for their share of the median asking rent in their region.84
- Compensates landlords for costs associated with their registration and ongoing engagement with the regulator.
- Covers the cost of additional tenancy security (e.g. minimum terms of two years).
- Reflects the landlord’s agreement to permit minor household modifications that bring the property in line with housing standards for new builds in the area.
Just like rent assistance, ideally this payment should be provided directly to the person enrolled in the NDIS.85
To receive the payment, the person who needs living and housing support should need to register their rental agreement with the NDIS Quality and Safeguards Commission. Registration would ensure that the NDIS Quality and Safeguards Commission can keep track of when there is more than one participant registered at an address, which could trigger an audit of quality and safety.
This recommendation differs from the NDIS Review recommendation to create a new Specialist Disability Accommodation category for people with intensive living supports who do not currently quality for SDA, to enable the review’s preferred one-to-three staff to residents ratio.86
A specific class of SDA housing that’s effectively designed to create new group homes risks entrenching the existing system for another generation.
Allocating this money to a fully portable stream would ensure it is not tied to a designated class of disability housing, and would increase the prospects of people with intensive needs living in ordinary homes in the community with Individualised Living Arrangements.
The cost of this payment is likely to be about $12,800 per person, or $187 million per year across all 14,600 people who currently receive Supported Independent Living but not Specialist Disability Accommodation.87 While the NDIS Review did not cost the alternative of a new Specialist Disability Accommodation payment, the lowest existing payment for a newly built group home is $53,772, and so even a greatly reduced reimbursement amount would cost the same or more than our proposal.88
Chapter 4: Improve planning and coordination
For disabled people to get better results from a wider range of housing and support options, they must have the time, help, and flexibility they need to plan their supports and navigate the system.
The way these processes currently work falls well short of what is needed, and the NDIA has not done enough to encourage innovation or to support people to make well-informed choices.
In the previous two chapters we outlined the alternative options that should be available and how existing services should be reformed. In this chapter we describe how planning, budget setting, and service coordination should work so that people who need intensive housing and living supports get more certainty, consistency, and specialist help from the NDIS.
The NDIS market also needs more help from government so that providers can step up to supporting people in new and different ways. The National Disability Insurance Agency must adopt a more proactive and strategic approach to stewarding the disability market, including by intervening directly to commission vital services, accelerate innovation, and support promising new approaches.
4.1 People don’t get enough help planning their housing and living supports
If you or a loved one needs housing and living support from the NDIS, you’re in for a bureaucratic nightmare. There is no dedicated pathway to these supports. That makes it difficult for people to navigate their way through the system, which often they have to do in a crisis.
Currently, the first step is to amass a raft of assessments and allied health reports showing how much support you need and how often.
Your documents are sent to the NDIS which centrally processes your application, usually without ever meeting you in person.
The NDIS is supposed to support people through this process, but actual guidance is limited. The NDIA contracts Local Area Coordinators to provide a few hours of (usually in-person) advice, but people frequently need to do a lot of legwork on their own.
Unless you have strong support from your family, it’s all too common for service providers to fill the gap. People will often contact a service provider during a crisis, and the provider will collate the required documents to apply for funding. The funding that results is then based
on what suits the kind of housing and support the provider offers, rather than what the person with a disability wants and needs.
It’s only once an application is approved that funding is provided to navigate the NDIS. People with complex packages receive funding for support coordination to help them spend their budget.
Support coordination is designed to give people in the NDIS agency over how they spend their money, but usually by this point a main support provider has already been chosen and so the opportunities for real choice are limited.
Despite an annual investment of more than $1 billion last year,89 the quality of support coordination is often poor, with little evidence specialist suppliers have risen to the challenge of helping people with intensive needs.90
Even if support coordination could help people explore more innovative options, NDIS funds are often already ear-marked for specific purposes before support coordination begins, so it’s difficult for people to use their budget in creative ways.
This process is the wrong way around. Funded supports are determined before disabled people have the opportunity to explore their options and consider what type of services will meet their needs and preferences.
NDIS packages are meant to be ‘consumer-directed’, but in practice 67 per cent of people in the NDIS say they find it difficult to get the care they need.91
To fix these problems, the NDIS needs to provide much more support and information to applicants before they choose their supports.
Participants should also be freed from prescriptive NDIS plans, so they can have real choice over how and where their money is spent.
4.1.1 Give people early access to a flexible budget before they start to plan
People should be able to get the NDIS housing and living budget they need quickly and easily, so that they can start to plan their supports.
The current process of listing every single need a person has and how it will be met, to create a budget from the ground up, is laborious and discourages innovation. To save time and increase fairness, Australia should adopt a system similar to the UK’s, where a standardised assessment of need is linked directly to eligibility and a funding system that provides a budget before planning commences.92
Amendments to NDIS legislation, proposed by the federal government in response to the NDIS Review, would enable this change. If the amendments are passed, people needing intensive housing and living supports should get priority during the transition to the new process, because they would stand to benefit the most from it.
There should be a single gateway to intensive housing and living supports. But the NDIA should also identify and carefully manage the group of people now getting less-intensive support but likely to
transition onto this pathway in future, for example due to family support arrangements becoming unsustainable.93 By focusing on the pipeline as well as eligibility, the NDIA could smooth demand pressure by funding supports that prevent, reduce, or delay entry.
Once assessed, people should get an indicative budget so they can start exploring what housing and living supports might suit them, with an understanding of the resources available to them. For most people who need intensive housing and living supports, allocation to one of three funding bands reflecting different levels of need should give them the scope and flexibility they need.
Our proposed funding bands, set out in Table 4.1, reflect our analysis of current costs for people using intensive housing and living services.
These bands are intended to be illustrative rather than prescriptive; there would need to be extensive consultation before the bands were finalised.94
The indicative budget that is provided should not be fixed, but rather the system should work like in the UK where final funding allocations are determined only after each individual’s plan is developed and agreed on.95 For example, the planning process might identify that an individual needs a bigger budget to cover a specialist item of assistive technology or a particular home modification.
Our proposal for funding based on need contrasts with the NDIS Review’s recommendation for a single benchmark, pegged to the default expectation of one-to-three staffing ratios of support workers and people who need intensive housing and living supports. While simple for funders, tethering to this ratio risks predetermining the service outcome and misses the opportunity to allocate funds to more innovative housing arrangements such as those discussed in Chapter 2.
By tethering funding to need rather than staffing ratios for group homes, and showing that proposed levels are sufficient to cover a range of arrangements, money could be used for a much greater variety of support. Our analysis of the costs of Western Australia’s Individualised Living Arrangements and the costs of typical packages of shared support within the current system suggests that the three funding bands we propose would capture most packages, without increasing overall costs.
The current funding and claiming categories of Supported Independent Living and Individualised Living Options should be ditched. The current long list of items in each person’s housing and living support budget should be replaced with a single dollar figure. And new, simplified pricing arrangements should be developed which can be used across service types.96
Table 4.1: Grattan’s proposed intensive housing and living funding bands
| Passive overnight | Active overnight | |
|---|---|---|
| Band 1 | $175,000 | |
| Band 2 | $230,000 | $280,000 |
| Band 3 | $340,000 | $410,000 |
Source: Grattan analysis.
This would give people and their providers more opportunities to use the money in ways that best suit their individual circumstances. The specifics of each person’s living arrangement should be recorded as part of approving the plan.
Funding that can be flexibly used within an overall budget determination for housing and living supports would help people to innovate and offers the potential of achieving greater value from the dollars available.
While most of a person’s living support budget should be flexible, Specialist Disability Accommodation funding should remain quarantined, because the SDA system is still maturing and SDA investors need predictability around returns.
4.2 Introduce specialist housing and living support navigators to help people make choices
Flexible budgets would enable people to think more creatively about their support, but they would also need help to understand their options and exercise real choice.
The NDIS should fund specialist housing and living navigators to help people develop their plans and navigate the system. The planning process should happen as close to the person and their community as possible. Navigators who understand local circumstances and have strong relationships with community organisations and providers will be best placed to help people with intensive needs get the right support.
While all people on the NDIS might eventually benefit from navigators, the need is greatest for those who require housing and living support. Navigators should work with two distinct groups: those identified as likely to need intensive housing and living supports in the future, and those who already do.
The navigators’ first job should be to help people to gather the information needed for the NDIA to allocate their funding. Once a person’s indicative budget has been set, this should be communicated to the local specialist navigator, who could work with the person and their chosen supporters to build a plan to meet their needs.
Navigators should not just help people find services, they should help people set goals and build knowledge and expectations (Box 4 on the following page lists a range of roles the navigators should play). This won’t simply be a matter of better matching supply and
demand. Successful navigation would raise the bar of low, entrenched expectations, and build new kinds of demand while working with the market to shape a more varied and individualised response to people’s needs.
The navigation service should be long term and have an emphasis on face-to-face engagement. It should ramp up at important life stages for the people it serves, such as when they are planning to move out of the family home for the first time. But the extent of a person’s engagement with their navigator should also be a matter of personal choice. It will be important that navigators not crowd out the role of family members, advocates, or peers, where a person has the skills and inclination to take on more of the legwork themselves.
Navigators would need time and resources to do their job well. They should have mixed caseloads that include people who are planning for the future as well as people who currently have intensive housing and support packages.
Caseloads should be set at a level that enables navigators to have frequent, meaningful interaction with the people they are helping, rather than navigators being available only in a crisis. Interaction should be
in-person wherever possible, because this group of people won’t be adequately supported through web-based or other remote service offerings.
Box 4: How specialist housing and living support navigators should help
The range of roles specialised navigators should play includes:
- Collecting information needed for assessment and budget setting;
- Helping people develop their own housing and living goals and build their understanding of what is possible;
- Helping to build and sustain people’s networks of informal supports;
- Helping people to understand local service market conditions, and opportunities within their local community;
- Supporting people to apply for social housing, and connecting people with local tenancy support organisations when needed; Supporting people to test alternative housing and support arrangements when they are considering making changes;
- Connecting people with providers and community groups, including advocacy organisations that can support people with decision making;
- Helping people connect to other mainstream or government services they may need in addition to NDIS supports;
- Collecting baseline information about the people in the service, including their current housing and support arrangements.
The NDIA should directly commission the specialist housing and living support navigators. The cost of the service should be partially offset by re-purposing funding for support coordination currently included
in plans for people with intensive in-home support needs, as well as a proportion of operating costs that currently go to fund Local Area Coordinators.
The NDIA will need tighter control than it has today for support coordination, over how this specialist service is designed and implemented, so it can eradicate conflicts of interest, more easily manage quality, and ensure the right amount of support gets to the right people.
4.3 The NDIA must do more to steer the market
Almost all of the NDIS’s funding goes to individual plans, with little opportunity for the NDIS to champion innovative support options. The NDIA does fund demonstration projects in housing and living, but these pilots have lacked direction and adequate funding.97
The new living support arrangements discussed in Chapter 3 on page 29 often require significant, long-term research and development funding, making it difficult for capital-constrained providers with short-term financial pressures to innovate.
Relying on the individual purchasing decisions of a high-needs group with low expectations is unlikely to spur market innovation. Like other markets for care and welfare services, sometimes referred to as ‘quasi markets’,98 the NDIS needs careful market stewardship.99
The Department of Prime Minister and Cabinet describes the role of market stewardship in the care and support economy as being ‘to ensure the market is delivering policy objectives, including by addressing market deficiencies or failures and by creating incentives that shape market behaviour towards desired outcomes’.100
This can be done by amplifying the voices of people using services, adjusting funding models, and intervening directly to plan and procure services where required to shape the market in response to changing needs and strategic goals, a process sometimes called ‘commissioning’.101
The NDIA needs to be a more influential steward and commissioner in the NDIS market, particularly as it relates to people needing intensive housing and living supports.102 The current light-touch approach, where price controls are the only direct intervention outside of thin markets, is not up to the job of delivering better housing and support options.103
4.3.1 NDIS regional hubs should lead the charge on innovation
NDIA market stewardship needs to be local. Attempts to shape markets from the Canberra bubble are unlikely to work.
The need for local co-ordination of innovative services is well- established in primary health. Primary Health Networks (PHNs) are given considerable local autonomy and resources to commission services in community health, spending more than $11.4 billion in 2021-22 alone.104
Experience from direct commissioning in the UK also attests that local intelligence in market management is a key ingredient for the success of new programs.105 Commissioning efforts that support local diversity in the organisations able to deliver individualised services to disabled people can also be a good thing, with community based organisations closer to the people they support often able to innovate more easily in how services are delivered.106
The NDIA should create a network of regional hubs mirroring the geography of PHNs, that can facilitate the growth of innovative NDIS services for their local communities. These hubs would provide a more localised workforce with the skills and capability to support market stewardship activities aligned to the NDIA central office’s strategic direction-setting, as described in Figure 4.1 on the following page.
Regional hubs should commission the specialist navigator workforce for their area, with the functions discussed in Section 4.2 on page 39. Navigators’ understanding of disability and local need, together with strong relationships with mainstream services, public housing, local governments, and providers, means they would be well placed to act as system stewards on their patch.107
The new regional hubs should be empowered with commissioning budgets, to plan and monitor system improvements and to build the capability of providers. The hubs should seed-fund innovation but also directly commission some services that have proved less suited to individualised purchasing.
The regional hubs should commission capacity building organisations that are skilled in working with individuals and families to develop novel arrangements.108 The hubs should also fund supports to help disabled people make decisions, such as peer support, microboards (as discussed in Section 3.1.2 on page 31), or Circles of Support.109
The specifics should be worked out with the local community in each region, and the commissioning intentions should be made public.
People with disability should be directly involved in advising the regional hubs, to ensure there is a golden thread from the issues they experience on their patch, through to regional stewardship, and onwards to direction setting by central agencies.
The NDIA should work with regional hubs to set system-wide priorities, coordinate multi-jurisdictional trials, evaluate local trials, and help spread programs that are particularly successful. This would include the NDIA establishing clear performance management, data
consistency and outcome collection systems for the new regional hubs, to ensure that people with disabilities living in all regions could expect high-quality regional stewardship.
Regional commissioning would enable the NDIA to create test-beds for innovation. Often providers will need to trial new approaches that are unproven in their operating environment, and predictable funding would ensure they are better able to take on the risk until funding from people’s individual plans can take over.
Figure 4.1: Under the Grattan plan, regional hubs would bridge the gap between the NDIS and Australians with disability
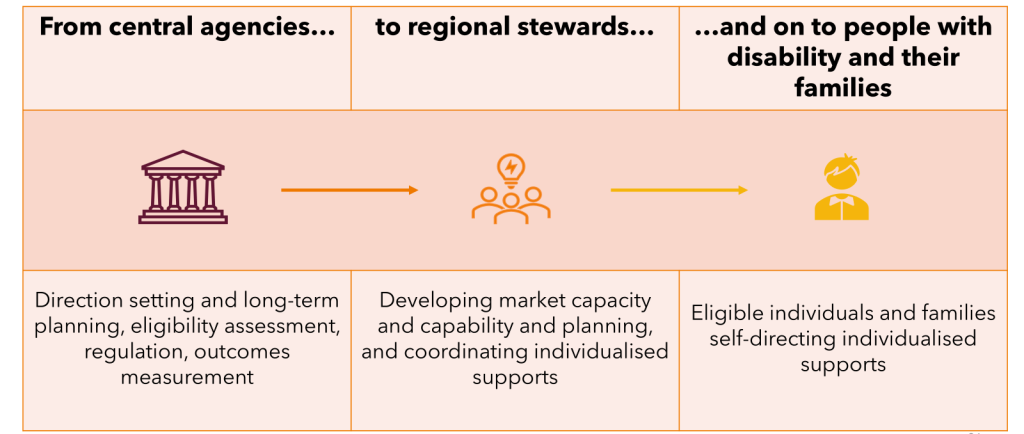
4.3.2 Regional offices should lead the transition away from group homes
Reducing the NDIS’s dependence on group homes should be a priority for the NDIA. A main focus of regional hubs’ commissioning activities should be to trial and spread promising alternative arrangements or test new ideas, starting with the approaches outlined in this report.
The NDIA should create a dedicated innovation fund to trial and spread individualised living arrangements and optimise the use of technology in delivering cost effective in-home supports.
Existing demonstration projects should be wound up into work plans for the new regional hubs.110 This would give providers clear guidance on the future direction of government policy, and would help innovators to develop new service blueprints for others to follow.
4.3.3 Regional offices will require significant investment
Enhanced planning, coordination, and market stewardship will come at a cost (see Table 4.2 for our estimated breakdown).
The government has already committed $20 million over two years to commence consultation and design of a new service navigation model, including specialist housing navigation.111 This should cover initial costs to establish regional offices, which will require significant implementation support to ensure new structures are set up for success. We estimate there will also be ongoing costs of about $700 million a year, which would be partially offset by redirecting about $310 million currently spent on support coordination for people with intensive needs, as well as a proportion of the operating costs that currently go to fund Local Area Coordinators.
The innovation fund and trials of new arrangements we are proposing will also require new investment of about $500 million over five years. This should be offset against the future costs of high-cost institutional support models being replaced by more cost-effective community-based living arrangements.
Table 4.2: Estimated costs of the Grattan plan for navigators and regional market stewardship
| Service type | Coordination hrs/yr | Total cost/yr |
|---|---|---|
| Coordination Level 1 | 48 | $120m |
| Coordination Level 2 | 72 | $206m |
| Coordination Level 3 | 108 | $308m |
| Coordination total | N/A | $634m |
| System management | N/A | $68m |
| Grand total | N/A | $702m |
requiring nine hours each month costed at specialised rates. To calculate the system management costs, we assume each of 31 regions around the country would need 20 staff on average to undertake market stewardship, at a cost of $110,000 per person with 40 per cent added for overheads.
Source: Grattan costings.
Chapter 5: Make governments accountable for better quality and safety
NDIS agencies need to take a far more active role in ensuring the quality and safety of services delivered to people who receive intensive housing and living supports.
Firstly, the NDIA should keep track of where each person with intensive needs is living, and keep this information up to date. Annual reports should be released that identify how many people are living at home with family, in their own home, in specialised housing, or in group homes sharing with others.
Secondly, any provider of living support should be subject to unannounced inspections to ensure the safety and quality of service provision. Specialist Disability Accommodation and group-home providers, and providers overseeing Individualised Living Arrange- ments, should be subject to advanced registration; disabled people who are self-directing their supports should register themselves.
5.1 All shared-accommodation providers should be subject to advanced registration
Group-home environments create a high risk of violence, abuse, and neglect, as detailed in Section 1.2.1 on page 9, and yet there is currently no requirement for these homes to be registered with the NDIS, unless they are registered SDA dwellings.
Consistent with the findings of the NDIS Review, advanced registration should be extended to all shared-accommodation settings (such as Supported Residential Services, boarding houses, and group homes), in addition to the services already designated as high-risk.
Where people choose Individualised Living Arrangements, these should also be overseen by a registered provider who helps develop the package, checks how it is working, and assists with resolving problems. The exception to this is where people with disability are self-directing their supports, in which case they should register themselves so that their formal and semi-formal supports are visible to the NDIA and the NDIS Quality and Safeguards Commission.112
Semi-formal supporters living in these arrangements should complete a worker screening check if a registered provider is overseeing the arrangement.
5.2 All shared accommodation providers should be subject to random inspections
Currently, providers that are required to register do so through a process that mandates third-party audit of their quality and safety, conducted at regular intervals. But a third-party audit is not enough to ensure the safety of people with intensive support needs.113
The nature of these services means that people are at a much higher risk. And yet these audits have been described by the sector as a ’paper-based’ exercise focused on ticking boxes rather than improving quality.114 The NDIS Quality and Safeguards Commission needs to have more oversight to adequately protect people. The Commission should also have the right (and duty) to enter all dwellings or homes where shared living supports (and other high-risk services) are provided, to inspect them and to check the welfare of people with disability.115
Inspections should be unannounced, or there should be only minimal notice given. Short- or no-notice Commission-led inspections are already performed for Hospitals and Aged Care, and high-risk disability services and settings should be no different.116
Inspections could be similar to those conducted in the UK, with inspectors observing the supports being provided, checking on the welfare of people with disability separate from staff and providers, inspection teams including people with disability, reviewing records, and documenting findings.117
Under-staffing is a problem for the Commission. We agree with the NDIS Review that the NDIS Quality and Safeguards Commission was not ‘set up for success’.118 Inspections are an important safeguard, and the Commission needs adequate staffing to conduct them. The important role of Community Visitor Schemes should be complimentary rather than in place of this formal regulatory role.
We estimate that, to visit enough homes to have a real impact, the Commission will require an extra $14m a year – about a 15 per cent increase in its yearly operational funding. This amount will be enough to ensure most group homes can be inspected as part of the registration process.
People with disability who self-direct their supports, who engage a variety of their own support staff, and have extensive informal support networks should be able to opt-out of the inspection process, where it is deemed that they are at low-risk of harm. While this arrangement will not be common, it will provide an outlet for the small number of people in this category whose concerns about the invasion of privacy that can occur from unannounced visits would outweigh any risks they face.
5.3 Publish quality and safety reports
The NDIS Quality and Safeguards Commission publishes no data on the quality of services delivered by individual providers, beyond the provider being deemed either compliant or non-compliant at the point of registration. There is little information available for people to decide which service might be right for them.
In contrast, the Aged Care Safety and Quality Commission publishes the full results of every audit conducted on aged care homes, enabling people to read in detail about the quality of services provided by a given facility.
The NDIS Quality and Safeguards Commission should publish reports with the certification of each registered provider of housing and living supports, marking their performance against the NDIS practices standards. These reports should be completed for each facility, rather than each provider, to ensure people can decide which facility suits their needs. The report should include a record of any complaints made against the provider in relation to the facility, including any compliance actions taken.
The NDIS should move over time from reporting on the activities conducted by providers and towards the results for people in the scheme. These reports may need to be published at a provider level to protect people’s privacy.119
While inspections should also be conducted of Individualised Living Arrangements, these reports typically would involve only one NDIS participant and therefore need only be circulated to that participant and would not need to be published. Registered providers of individualised arrangements should be subject to inspections with some notice, so that visits can be arranged to the homes of disabled people using their services.
5.4 Report on the transition from group homes
The Disability Royal Commission recommended a 15-year transition away from group homes and towards more innovative living options. Some parts of these reforms can be achieved much quicker, as we described in Chapter 3 on page 29. But the NDIS currently lacks the data to measure who is in a group home, who is in a share-house, and who is in a more individualised living arrangement.
The NDIA should collect housing data for all people who receive NDIS supports. Data should include the number of people in a household, the type of household, and its location.
A specific priority should be to fill the current data vacuum around the circumstances of people living in legacy group homes. The NDIS should commission organisations funded through the National Disability Advocacy Program to establish a baseline picture of these services and their residents, to assist with transition planning.
The NDIA should aim for 100 per cent data coverage by the end of 2026. The data standard for type of household should include detailed information about different living arrangements so it is clear which homes are ‘group homes’, which are more share-house type residences and, when someone has an Individualised Living Arrangement, what are the key components of the package.
The NDIA should then publish a yearly report detailing progress on the transition away from group homes, including the number of residents entering a group home each year, the number leaving, the number entering more innovative options, and the progress of trials of more innovative options.
The NDIA should set interim yearly targets so that progress against these targets can be measured towards a goal of full transition within 15 years.
5.5 Report on results
There is no guarantee that the shift away from group homes will improve the lives of people with intensive needs. Research has shown cases of low-quality care and abuse in a variety of living environments.120 But the need for change is crystal clear and uncertainty about the future should not prevent progress or justify yet more inertia.
Rather, as people transition from group homes into alternative housing, it will be essential to see how their lives have changed and what improvements or problems there have been, so that reforms can be refined on the basis of experience.
The NDIS already collects data on participants’ outcomes across eight domains, including health, choice and control, housing, and social participation. These data are then used to produce reports that are broken down by age group, but not by housing status.
The NDIS needs to start recording outcomes specifically for people living in group homes, Specialist Disability Accommodation housing, and other supported living environments, so the impact of innovative arrangements can be measured. This data should shed light on the experience of people living in group homes, who are hard to identify in the data and unlikely to fill-out the surveys on which this reporting is primarily based. Measuring outcomes in this group takes care, and some strategies are discussed in Box 5 on the next page.
The NDIS Review recommended that the NDIA develop a series of bundled payments which include some outcome-related component for shared accommodation providers, linked to these outcomes.
However as an interim step, the Review recommended incentives be linked to consumer satisfaction.121 Given reliable outcome measures will take time to validate, it’s reasonable to have interim measures.
But satisfaction is an extremely difficult measure to validate, and it would be far preferable to rely on process metrics instead in the short-term – such as providers producing evidence of progress away from group-home care models.
5.6 Develop specific practice standards for Individualised Living Arrangements and shared accommodation
NDIS practice standards give the sector concrete expectations on what care is needed in order to achieve NDIS registration. Practice standards are considered as part of the audit process that registered providers must complete.
In January 2023 the NDIS Quality and Safeguards Commission completed an own-motion inquiry into aspects of shared accommoda- tion. The paper included research into what standards are expected in shared accommodation and how practice standards could be developed to ensure providers are up to scratch.122
These standards now need to be developed so that there are clear and shared expectations about quality and safety.
We recommend that separate practice standards are also built to codify quality and safety in Individualised Living Arrangements. Generic standards won’t work across all services, and a lack of clarity around safeguarding responsibilities in these arrangements is a barrier to their wider adoption.
Box 5: How to measure performance and results of housing and living supports
The NDIS needs to take the time to measure performance and outcomes for people using housing and living supports across many domains.
To be effective, outcomes data collection must also consider innovative ways to reach people with intensive needs and cognitive impairments. Some measurement frameworks are designed specifically for people who struggle to complete surveys.a
Several guides exist which are specific to particular types of service, such as hostsb, and work by Curtin University provides a useful framework for reviewing what is and is not working across a range of individualised arrangements.c
The Summer Foundation has also done useful work to measure individual outcomes for people with disability and complex needs moving into newly individualised apartments in the community, measuring outcomes across four domains: emotional wellbeing, care and support needs, overall health, and community participation.d
Data on outcomes for people in the NDIS need to be collected in a longitudinal manner, so that outcomes for people who transition to different living arrangements can be compared.
a. Bigby et al (2014).
b. Such as the UK’s Shared Lives Plus practice standards: Shared Lives Plus (2015).
c. Cocks et al (2017).
d. Douglas et al (2023).